image courtesy of American Heart Association
Differential Diagnosis I
Transient Ischemic Attack (TIA)
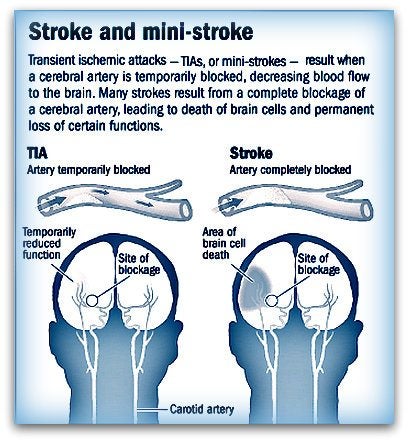
image courtesy of braininjury-explanation.com
Rationale:
A TIA is the result of localized ischemia causing neurological deficits that resolve in no more than one hour. Clinical manifestations such as weakness, altered mental status, and headache, often mimic a stroke. Patient has a history of a previous TIA but at this point her symptoms have lasted greater than one hour. About 3-17% of patients who have a TIA will experience a stroke in the next 90 days. So, while it is a differential diagnosis it is also a risk factor/indicator for stroke. TIA is differentiated from stroke with resolution of symptoms and imaging, such as MRI, to rule out stroke (McCance & Huether, 2018).
Differential Diagnosis II
Hypoglycemia

image courtesy of Diabetes Self-management.com
Rationale:
Hypoglycemia is defined as a blood glucose level of less than 70 mg/dL in adults. Clinical manifestations include headache, confusion, tremors, weakness, fatigue, and seizures. Patient is at risk for hypoglycemia due to diabetes diagnosis and insulin use. Hypoglycemia is easily and quickly ruled out by blood glucose check and treatment as indicated (McCance & Huether, 2018). The patient’s blood glucose was 163 on arrival to the ED so hypoglycemia is ruled out as a differential diagnosis.
Differential Diagnosis III
Seizure/Postictal Phase

image courtesy of Marshfield Clinic
Rationale:
The postictal phase is the period of time immediately following an epileptic seizure and may last from a few minutes to hours. Clinical manifestations often mimic a stroke and include headache, confusion, memory loss, paralysis, aphasia, and lethargy. However, patient does not have a history of seizures and there was no witnessed seizure activity. Labs can help identify any systemic conditions that may cause seizures. MRI and EEG can analyze the brain and brain activity for evidence of seizures (McCance & Huether, 2018).
Differential Diagnosis IV
Subdural Hematoma (SDH)

Image courtesy of emedicinehealth.com
Rationale:
A SDH is a pooling of blood between the brain and the dura most often caused by trauma. It may be acute, developing in hours, or chronic, developing over the course of a few weeks. Clinical manifestations include headache, confusion, lethargy, weakness, and dysphasia. The patient is at an increased risk for a traumatic brain injury due to a history of frequent falls. Family states that there has been no recent, witnessed fall but there is still the possibility that the patient had a fall that was not witnessed by family. If present, a SDH will be visible on a CT scan (McCance & Huether, 2018).