(DiGiovanna, A. G; 1999)
Cerebrovascular accidents, also known as strokes, happen when the blood supply becomes occluded in part of the brain. They can be classified as either ischemic, hemorrhagic, or cryptogenic. In ischemic strokes blood supply can be occluded for three different reasons, a vascular occlusion by either an embolus or thrombi, a gradual vessel occlusion, or a stenosed vessel (McCance & Huether, 2019). In ischemic strokes or cerebral infarctions, the arterial blood flow that leads to the brain is obstructed and can be classified as ischemic infarcts or hemorrhagic infarcts. This can be from transient ischemic attacks, thrombotic strokes, embolic strokes, lacunar strokes or hemodynamic strokes. In an ischemic infarct, the area that is affected becomes pale, soft, and swollen. This eventually leads to necrosis of the brain tissue which creates a cavity that is surrounded by glial scarring (McCance & Huether, 2019). If an occlusion of a cerebral artery occurs, branches of connecting arteries can partially maintain blood supply to prevent cell death (McCance & Huether, 2019). In hemorrhagic infarcts leaking vessels create a bleed when fragments from an emboli resolve and reperfusion starts (McCance & Huether, 2019).
There are many different types of ischemic strokes that can occur in the human body. Transient ischemic attacks are dysfunctions in the brain that cause ischemia for about one hour. Transient ischemic attacks can eventually lead to a stroke within 90 days if not fixed. Individuals experiencing a TIA may have weakness, numbness, loss of vision or balance, a severe headache, or confusion (McCance & Huether, 2019). In thrombotic strokes a thrombus is formed inside the vessels that feed the brain or intracranial vessels and a part of that clot detaches, travels up to the brain, occludes blood flow, and causes ischemia (McCance & Huether, 2019). Embolic strokes start in the outside of the brain, either in the heart, aorta, or common carotid artery where a thrombus is formed. Parts of that thrombus breaks off and causes an obstruction usually in small brain vessels causing ischemia (McCance & Huether, 2019). In embolic strokes the embolus can completely occlude the vessels or have pieces that remain in vessels which can lead to a second stroke because the embolus is still there (McCance & Huether, 2019). In lacunar strokes there is edema or inflammation to the wall of an artery and leads to ischemia. They mostly occur in the basal ganglia, internal capsules or the pons. Lastly, in hemodynamic strokes there is inadequate blood supply to the brain caused by either cardiac failure, pulmonary embolism or bleeding (McCance & Huether, 2019).
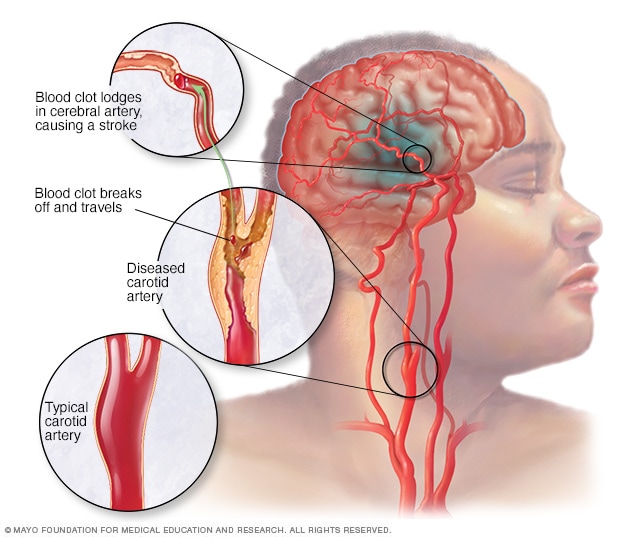
(https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113)
In a hemorrhagic stroke or spontaneous intracranial hemorrhage, bleeding happens in the brain tissue causing a mass of blood due to leaky vessels or bursting aneurysm (McCance & Huether, 2019). In both ischemic and hemorrhagic strokes, the decrease in blood supply causes ischemia which can eventually cause death of the tissue or infarction. There are two types of hemorrhages that can occur from a hemorrhagic stroke, subarachnoid hemorrhage and intracerebral hemorrhage. Subarachnoid is a bleed that occurs between the brain and the dura while an intercerebral bleed occurs actually in the brain parenchyma. Brain tissue that is near the bleed can start to become compressed and can be displaced causing ischemia, edema, increased intracranial pressure, and necrosis (McCance & Huether, 2019). Hemorrhagic strokes can range in all different sizes which can determine how much edema and necrosis there will be. They can be classified as massive, small, slit, or petechial (McCance & Huether, 2019). In a massive cerebral hemorrhage, there will be a significant amount of edema which can lead to death.
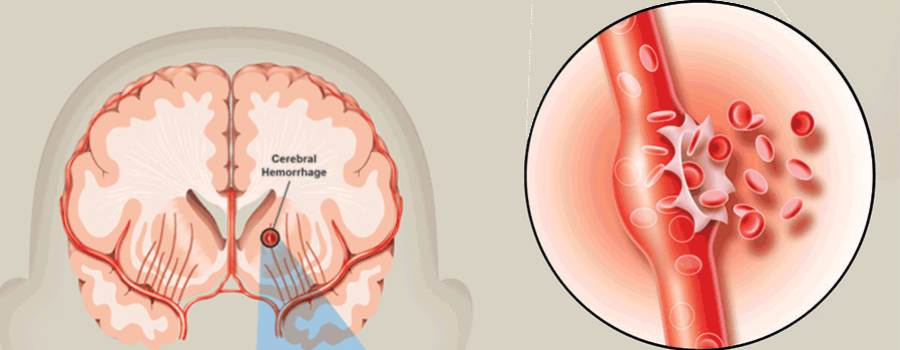
(https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113)
Symptoms of a stroke happen fast and can range from mild to severe depending on how large the stroke is and what kind of stroke the person is experiencing. In a thrombotic or embolic ischemic stroke, the symptoms a person may experience varies depending on what artery in the vein is involved (McCance & Huether, 2019). A person may loose sensory and motor function on the opposite side of where the stroke happened in the brain making it contralateral or on the same side as the stroke making it ipsilateral. In a hemorrhagic stroke a person may experience a horrible headache that leads to unresponsiveness, a headache but a person remains conscious or a person can immediately become unconscious. They can also have numbness and tingling, speech issues, weakness or paralysis. In some cases, if the hemorrhage is just in the subarachnoid space, a person may not experience any symptoms at all (McCance & Huether, 2019).
Upon observations of possible symptoms or clinical manifestations of a stroke, as detailed throughout this website, imaging tests are used to identify and diagnose. The key criteria for diagnosis are a CT of the head and MRI of the brain. These tests can confirm if there is a stroke, and determine what type of stroke so the practitioner can appropriately treat the individual (McCance & Huether, 2019).