Differential Diagnosis I
Urinary Tract Infection – Acute Cystitis
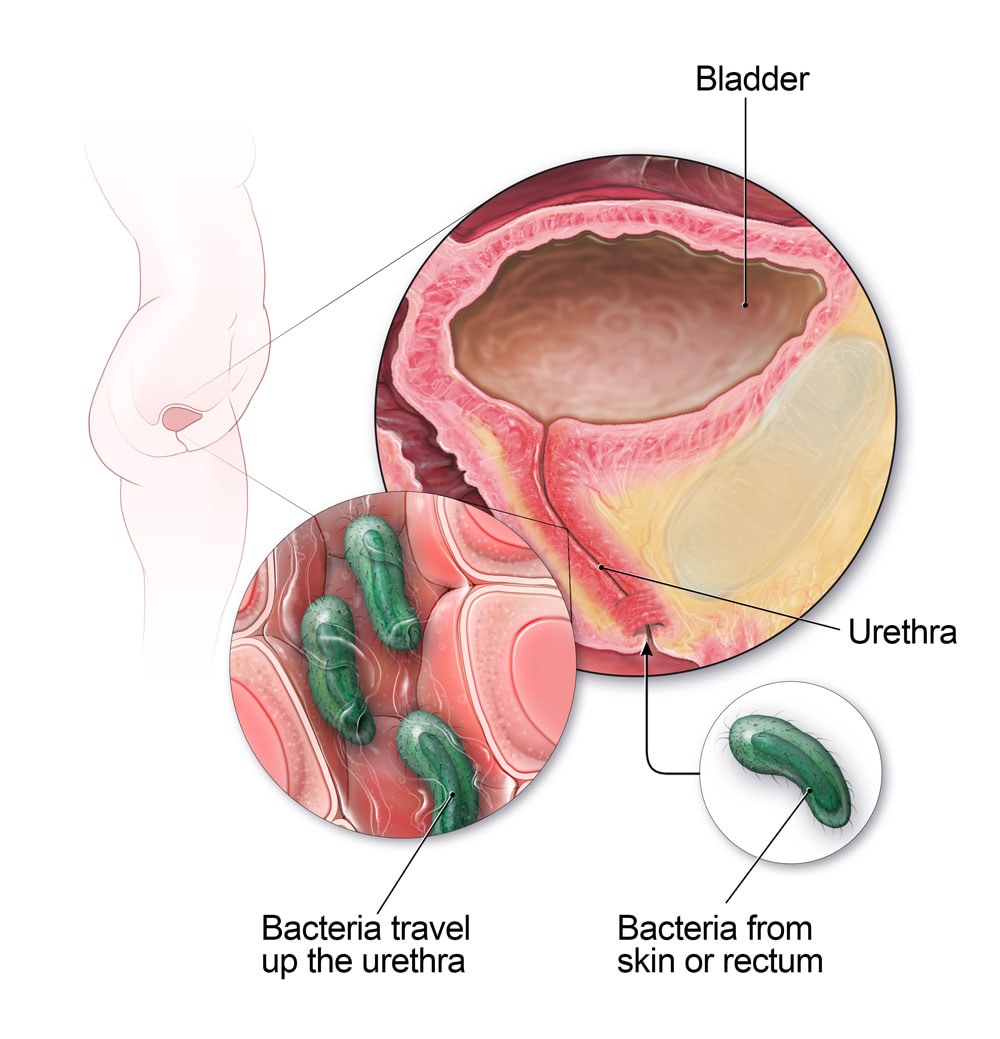
Figure 1. Urinary Tract Infection. (CDC, 2019)
A urinary tract infection (UTI) is inflammation of the urinary epithelium and can occur anywhere along the urinary tract, including: the urethra, bladder, ureter or kidney. Individuals at risk for UTI are premature newborns, sexually active and pregnant women, individuals with indwelling catheters, and individuals that are diabetic, have neurogenic bladder, or urinary tract obstructions. UTIs may occur alone or in association with pyleonephritis, prostatitis, or kidney stones. Acute cystitis, a type of UTI, is inflammation of the bladder and the most common type of UTI. Acute cystitis occurs when there is bacterial contamination of sterile urine through the backwards movement of gram negative bacilli from the gut into the urinary tract. The most common infecting microorganisms of acute cystitis are Escherichia coli (80% to 85%) and Staphylococcus saprophyticus (10%). This bacterial contamination leads to infection of the urinary tract and therefore causes an inflammatory response.
Less serious clinical manifestations of acute cystitis include: frequency, urgency, dysuria, and suprapubic or low back pain. Inflammatory edema in the bladder wall stimulate stretch receptors, initiating the symptoms of bladder fullness with small volumes of urine; this causes the symptoms of urgency and frequency of urination. More serious clinical manifestations include hematuria, cloudy or foul smelling urine, and flank pain. Diagnosis is made based upon urine culture with sensitivity. Treatment includes prescription of a microorganism-specific antibiotic. (McChance & Huether, 2019, p. 1255-1256).
Rationale:
E.S. is at an increased risk for developing a UTI due to his age being a type II diabetic. He is also endorsing symptoms of frequency, urgency, and lower back pain which provide rationale for this diagnosis.
However, there are a few reasons why E.S. may not be suffering from a UTI. First, he is not at high risk of developing a UTI due to him being male. Males are at lower risk of developing UTIs due to them having anatomically longer urethras, therefore infectious bacteria must travel a longer distance to reach the bladder. He has been experiencing a insidious progression of urinary tract symptoms, and one would expect if he had a UTI that his symptoms would have had a more acute onset. On top of that, he was recently treated for UTI, completed his course of antibiotics, and his urinary symptoms were unresolved. Finally, he is also not complaining of dysuria, which would be expected symptom with UTI. These reasons provide rationale for why E.S. could potentially not have a UTI. (McChance & Huether, 2019, p. 1255-1256).
Differential Diagnosis II
Benign Prostate Hyperplasia

Figure 2. Prostate and Benign Prostatic Hyperplasia. (The Mayo Clinic, 2018)
Benign Prostate Hyperplasia (BPH) is the enlargement of the prostate gland. As the prostate gland enlarges, prostate tissue begins to compress the urethra which causes increasing frequency of lower urinary tract symptoms. Prevalence among U.S. men older than 70 years of age or older is 90%. BPH begins in the periurethral glands of the prostate. The prostate slowly enlarges as nodules form and grow, and glandular cells enlarge. The development of BPH occurs over a prolonged period, and changes in the urinary tract are slow. Current causative theories of BPH focus on levels and ratios of endocrine factors such as androgens, estrogens, gonadotropins, and prolactin. Changes in the balance between autocrine/paracrine growth stimulatory and growth inhibitory factors are also thought to be causative theories of BPH.
Clinical manifestations include urgency, hesitancy, decreased force of urinary stream, and urinary retention. Hematuria, bladder or kidney infection, hydronephrosis, acute urinary retention, and renal insufficiency are common complications of BPH. Diagnosis is made from medical history, physical examination, and urinalysis. Digital rectal exam and PSA can be completed to determine the presence of hyperplasia, however measurement of PSA level alone cannot diagnosis BPH as PSA levels can be elevated in both BPH and prostate cancer. (McChance & Huether, 2019, p. 846-847).
Rationale:
E.S. is at increased risk of developing BPH due to his age of 71 years. He is demonstrating symptoms of urgency, hesitancy, urinary retention, and hematuira – all common symptoms and complications of BPH. Also, his symptoms have progressed over a longer period of time, which align with a BPH diagnosis.
However, one symptom that is displaced in this diagnosis is that E.S. is complaining of unremitting lower back pain. Lower back pain is not a clinical manifestation or even a common complication of BPH. (McChance & Huether, 2019, p. 846-847).
Differential Diagnosis III
Prostatitis – Acute Bacterial Prostatitis (ABP)
Prostatitis is inflammation of the prostate. In acute bacterial prostatitis (ABP), there is an acute ascending infection of the urinary tract that causes an inflammatory response. The prostate in turn becomes enlarged, tender, firm, or boggy. ABP tends to occur in men between the ages of 30-50, but is associated with BPH in older men. Clinical manifestations are similar to UTI: fever, dysuria, urgency, hesitancy, nocturia, and urinary retention. Some individuals also experience lower back pain, painful ejaculation, and rectal pain. Diagnosis can be made with palpation of the prostate; which reveals it to be enlarged, tender, firm and warm to the touch and also urine culture with sensitivity. ABP is most commonly caused by gram negative bacteria Enterobacteriaceae and Enterococci species. Treatment includes antibiotics. (McChance & Huether, 2019, p. 848-849).
Rationale:
E.S. is demonstrating symptoms of urgency, hesitancy, nocturia, urinary retention, and lower back pain which provide rationale for this diagnosis.
E.S. is not at risk for ABP due to his age of 71 years, as ABP tends to occur in men between the ages of 30-50. Also, his urinary tract symptoms have been progressive, he is afebrile, and not showing signs of acute infection which would be expected with ABP. (McChance & Huether, 2019, p. 848-849).
Final Diagnosis
Prostate Cancer

Figure 3. Prostate Cancer. (The Mayo Clinic, 2017)
Prostate cancer is cancer of the prostate gland. Across all age ranges, African American men have an increased risk of developing prostate cancer and are twice as likely to die of prostate cancer compared with other men in the United States. Prostate cancer often does not show any signs or symptoms until it is advanced. The first manifestations normally seen are due to bladder outlet obstruction: slow urinary stream, hesitancy, incomplete emptying, frequency, nocturia, and dysuria. Local extension of prostatic cancer can also obstruct the upper urinary tract ureters as well. Unlike the symptoms of BPH, symptoms of prostate cancer are progressive and do not remit. Symptoms of late disease include bone pain at sites of bone metastasis, edema of lower extremities, enlargement of lymph nodes, enlargement of the liver, development of pathological fractures, and altered mental status associated with brain metastases.
Screening for prostate cancer includes digital rectal exam (DRE), prostate-specific antigen (PSA) blood tests, and transrectal ultrasound (TRUS). The most significant test used in diagnosis and management of prostate cancer is the measurement of PSA. DRE may detect early prostatic carcinomas but has low sensitivity and specificity. Diagnosis is confirmed via tissue biopsy. Other scans may be utilized to determine metastasis. (McChance & Huether, 2019, p. 857-858).
Rationale:
There are multiple reasons to suspect the diagnosis of prostate cancer for E.S.. First and foremost, he is at an increased risk of developing prostate cancer due to his ethnicity and his family history of prostate cancer in his father. He is demonstrating progressive and unremitting urinary tract symptoms of hesitancy, incomplete emptying, frequency, and nocturia. He is also complaining of worsening lower back pain, which may be an indicator of the development of bone metastasis. These reasons provide rationale for this diagnosis. (McChance & Huether, 2019, p. 857-858).