Correct Diagnosis/Differential Diagnosis I: Allergic Rhinitis
Rationale:
Patients with allergic rhinitis may experience clinical manifestations that affect the nasal mucosa, eyes, respiratory tract, and skin. The nasal mucosa often appear inflamed and swollen, but pale in color (Honan, 2019). Congestion in the nose occurs due to the swollen nasal conchae and excess production of mucus (Honan, 2019). The excess mucus may present as clear drainage with a runny nose, headache from accumulation of mucus in the sinuses, and an itchy throat as mucus drains down the respiratory tract. Inflammation of the eyelid membrane linings result in a red eyelid appearance known as conjunctivitis (McCance & Heuther, 2019). In some cases of allergic rhinitis, the airway may be affected through constriction of the bronchi. The skin may also be affected through the development of urticaria, or hives (McCance & Heuther, 2019). Manifestations of allergic rhinitis typically are persistent and vary according to season (Honan, 2019). Difficulty sleeping, fatigue, and irritability can also be manifestations of allergic rhinitis (Honan, 2019). Clinical manifestations of allergic rhinitis typically remain until the allergen is removed. Among the most common co-morbidities affiliated with prolonged and untreated allergic rhinitis are the following: allergic asthma, chronic nasal obstruction, chronic otitis media with hearing loss, anosmia, and the formation of dental deformities in children (Honan, 2019). To prevent the development of these serious complications later in life, a diagnosis and treatment regimen should be implemented early, when clinical manifestations first appear (Honan, 2019).
B.B.’s clinical presentations are consistent with this description. B.B. has persistent sneezing, runny nose, congested nose, watery and itchy eyes, red conjunctiva, sinus tenderness on palpation, itching on the roof of the mouth, and nasal mucosa that is pale and swollen. The patient’s mother also reported that her daughter is not sleeping well and seems fatigued most days. B.B. does not, however, appear to have any airway obstruction or urticaria. Some common environmental and seasonal allergens that trigger allergic rhinitis include dust mites, cockroaches, trees and grasses, pollen, mold, and animal dander (Eggleston, 2001). B.B. and her mother are living in a home that is older and may contain some of the common allergens described. The relocation to the countryside may also have exposed B.B. to new outdoor allergens, such as trees, grasses, and pollen. B.B.’s signs and symptoms are reportedly the worst when she wakes up in the morning (after sleeping with the windows open and a running fan) and when she plays outside. Symptoms caused by environmental allergens vary by season depending on the allergen that the patient is allergic to, but a common allergy period is during the spring (WebMD Allergies Health Center, n.d.), which is when B.B. is experiencing her symptoms.
Figure 1. Allergic rhinitis symptoms (Chun, n.d.).
Diagnostic Testing:
There are a variety of diagnostic tests that would be valuable to confirm that B.B.’s symptoms are a result of allergic rhinitis. One laboratory test may involve assays to detect IgE antibodies in the blood (McCance & Heuther, 2019). If the laboratory serum assay for IgE antibodies indicates that an allergic reaction is occurring, then follow-up skin or serum tests to determine the specific allergens will further clarify the allergic triggers (Honan, 2019). An alternative method may be a radioallergosorbent blood test which detects for specific IgE antibodies in the blood caused by the immune system’s response to allergens (Shah & McGrath, 2012). Furthermore, allergic rhinitis has been associated with multiple gene mutations of cytokines that regulate IgE synthesis (McCance & Heuther, 2019), so genetic testing may also be valuable to determine a diagnosis of allergic rhinitis.
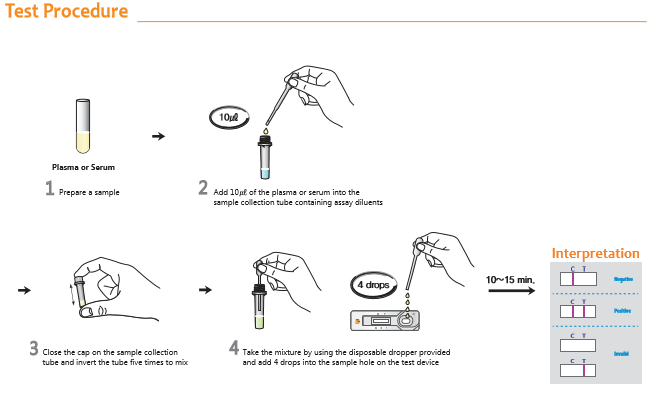 Figure 2. Assay test procedure steps for IgE antibody (QBIOTECH, 2014).
Figure 2. Assay test procedure steps for IgE antibody (QBIOTECH, 2014).
Differential Diagnosis II: Viral (Non-Allergic) Rhinitis
Rationale:
Viral or non-allergic rhinitis (also known as the “common cold”) is manifested through signs and symptoms similar to the ones described for allergic rhinitis. Serous nasal drainage and congestion, sneezing, headache, fatigue, sore throat, and itchy nose, roof of mouth, and eyes are some signs and symptoms similar to those experienced with allergic rhinitis (Honan, 2019). The nasal mucosa of patients with viral rhinitis is typically swollen and red due to hyperemia, or excess blood supply to the area (Honan, 2019). Viral rhinitis also usually involves a low-grade fever, muscle aches, chills, and a cough (Honan, 2019). The duration of signs and symptoms for viral rhinitis are usually only 5-7 days (Jones, 2019). Viral rhinitis affects 40% of children and is the most frequent viral infection in the general population (Honan, 2019).
B.B. does have some signs and symptoms that are consistent with viral rhinitis, including her persistent sneezing, runny nose with serous drainage, congested nose, watery and itchy eyes, red conjunctiva, sinus tenderness on palpation, and itching on the roof of the mouth. However, the patient has a nasal mucosa that is pale instead of red. The pale nasal mucosa is more consistent with an assessment finding for allergic rhinitis (Honan, 2019). Furthermore, B.B. has not reported any signs or symptoms of a low-grade fever, muscle aches, or chills. While viral rhinitis signs and symptoms usually only occur for 1-2 weeks, B.B. has been experiencing her clinical manifestations for much longer over the past few months.
 Figure 3. Symptoms of a common cold (Tharu, 2016).
Figure 3. Symptoms of a common cold (Tharu, 2016).
Diagnostic Testing:
The diagnosis process for viral or non allergic rhinitis begins with an assessment of current symptoms followed by the process of ruling out other potential causes, including allergies and problems of the sinuses (Mayo Clinic, 2019). The symptoms of allergic and nonallergic rhinitis can often resemble one another. To differentiate the diagnoses, providers may utilize specific tests discussed above to determine if the clinical manifestations are caused by allergies (Mayo Clinic, 2019). In addition, further evaluation of the nasal septum and inferior turbinates may be necessary if a patient is presenting symptoms commonly associated with rhinitis but have the potential to be sinus related (Shah & McGrath, 2012). In this instance, a nasal endoscopy or computerized tomography are imaging tests that can provide a greater insight into the nasal passages and sinuses for review (Mayo Clinic, 2019). A viral nonallergic rhinitis diagnosis is confirmed when the patient has been ruled out for alternative causes, especially allergens or bacteria (Mayo Clinic, 2019).
 Figure 4. Image of a nasal endoscopy (Nucleus Medical Media, n.d.).
Figure 4. Image of a nasal endoscopy (Nucleus Medical Media, n.d.).
Differential Diagnosis III: Acute Bacterial Rhinosinusitis
Rationale:
Acute bacterial rhinosinusitis involves signs and symptoms of nasal congestion, headache, and facial pain (Honan, 2019). Inflammation occurs in the nose and is accompanied by excessive and thick mucus that fills the sinus cavities (Honan, 2019). Fever and fatigue are also likely present (Honan, 2019). The nasal drainage for acute bacterial rhinosinusitis is typically cloudy and purulent with yellow or green color (Honan, 2019). Bacterial organisms are responsible for causing 60% of rhinosinusitis cases (Honan, 2019). There are a variety of bacterial organisms that may cause acute bacterial rhinosinusitis, most commonly including Streptococcus pneumoniae, Haemophilus influenzae and Moraxella catarrhalis (Cleveland Clinic, n.d.). Most cases of acute bacterial rhinosinusitis occur after acute viral rhinitis (Cleveland Clinic, n.d.). Symptoms that last longer than 10 days after the initial onset of symptoms affecting the upper respiratory systems may indicate acute bacterial rhinosinusitis (Honan, 2019). Symptoms of acute bacterial rhinosinusitis may also become worse over time (Honan, 2019).
B.B. has some signs and symptoms that are consistent with acute bacterial rhinosinusitis, including nasal congestion, headache, and sinus tenderness on palpation. The patient’s nasal drainage is a clear color, however, which is not consistent with the purulent and colored drainage normally seen in acute bacterial rhinosinusitis. The symptoms for acute bacterial rhinosinusitis typically last longer than 10 days, which is consistent with B.B.’s duration of signs and symptoms over several weeks. B.B. has not, however, noticed any signs of fever. The patient also has not reported any worsening of symptoms after initial improvement.
 Figure 5. Symptoms of rhinosinusitis (CORE EM, n.d).
Figure 5. Symptoms of rhinosinusitis (CORE EM, n.d).
Diagnostic Testing:
The first steps to determine if the rhinitis is caused by a bacterial infection are to rule out the possibility of allergic rhinitis and to gather patient history information regarding the duration of symptoms and description of nasal drainage. The standard for diagnosing acute bacterial rhinitis is a sinus puncture and culture of the aspirate. This allows the provider to determine if the symptoms are due to bacteria, and it also allows the health care provider to determine what bacteria is causing the infection so that an appropriate antibiotic can be prescribed (Lau,1999). This is not commonly performed though due to the fact that it is expensive, invasive, and not practical. Often a diagnosis is confirmed through patient history and physical examination presenting purulent nasal drainage, nasal obstruction, and/or facial pain/pressure that exists for more than 10 days without improvement, or if within 10 days these symptoms worsen over time (American Academy of Family Physicians, 2015).
 Figure 6. Completing a sinus puncture and collection of aspirate (Drtbalu, 2018).
Figure 6. Completing a sinus puncture and collection of aspirate (Drtbalu, 2018).
Differential Diagnosis IV: Immotile Cilia Syndrome (Ciliary Dyskinesis)
Rationale:
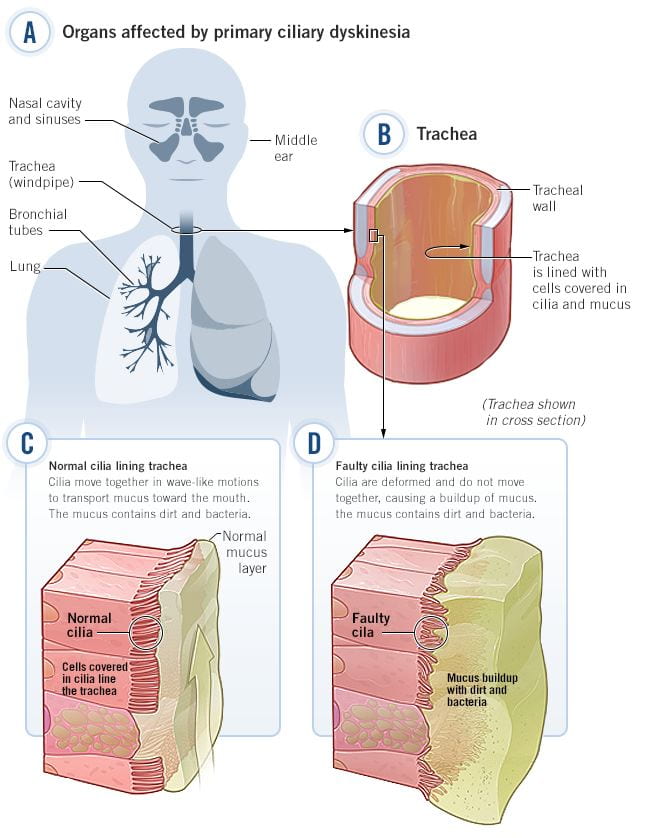
Immotile Cilia Syndrome (Ciliary Dyskinesis) is characterized by chronic respiratory infections caused by inherited impaired cilia function and structure. Ciliary Dyskinesis is an autosomal recessive inherited disorder (National Institute of Health, n.d.). Cilia are hair-like structures that help move particles and fluid through the respiratory tract and other body structures. The cilia that line the respiratory tract help to move mucus and microorganisms from the airway. Without proper cilia function, chronic respiratory tract infections occur. Patients with Immotile Cilia Syndrome typically have year-round nasal congestion and a chronic cough (National Institute of Health, 2019). Common signs and symptoms of Immotile Cilia Syndrome that involve the respiratory tract include chronic runny nose with mucus and pus discharge, nasal congestion, middle ear infections, coughing, and breathing problems (National Institute of Health, n.d.). Onset of symptoms occurs shortly after birth during the newborn stage (National Institute of Health, n.d.).
B.B. has some signs and symptoms that are consistent with Immotile Cilia Syndrome, including runny nose and nasal congestion that lasts at least 3 weeks. The patient’s onset of symptoms does not match the onset timing of symptoms though for Immotile Cilia Syndrome, as the patient onset of symptoms occurred 3 months ago as a 12 year old rather than as a newborn child typical with Immotile Cilia Syndrome. Furthermore, B.B. has not reported any signs or symptoms of persistent ear infections, cough, or breathing problems commonly associated with Immotile Cilia Syndrome.
Figure 7. Impact of primary ciliary dyskinesia on respiratory system (Circassia, n.d.).
Diagnostic Testing:
Health care providers would first assess for symptoms caused by rhinitis. If rhinitis diagnostic testing comes back negative, then this alternative diagnosis of Immotile Cilia Syndrome should be explored. Screening for suspected immotile cilia syndrome involves assessing nasal nitric oxide levels, which are low in patients with Primary Ciliary Dyskinesis (Lucas et al., 2014). Additional diagnostic testing includes a cilia structure assessment using transmission electron microscopy (Lucas et al., 2014). Ciliary beat frequency testing is also explored for diagnostic testing (Lucas et al., 2014). Furthermore, suspected Immotile Cilia Syndrome is confirmed or ruled out by genetic testing. There are over 1,000 genetic tests currently in use (National Institute of Health, 2019). Methods for using genetic testing include molecular genetic tests, chromosomal genetic tests, and biochemical genetic tests (National Institute of Health, 2019).
Figure 8. Genetic testing (Saey, 2018).