URINARY TRACT INFECTION – ACUTE CYSTITIS
URINARY TRACT INFECTION PATHOPHYSIOLOGY
DEFINITION:
- It is an inflammation of the urinary epithelium usually caused by bacteria from gut flora.
- It can occur anywhere along the urinary tract (urethra, bladder, ureter, kidney).
- UTI may occur alone or with pyelonephritis, prostatitis, or kidney stones.
NORMAL PROTECTIVE FACTORS / NORMAL FUNCTION OF URINARY TRACT SYSTEM:
-
Host defense mechanisms exist to maintain sterility and prevent UTI
-
Complete bladder emptying during micturition
-
Acidic pH
-
High urea concentration
-
Presence of uromodulin and uroepithelium mucous secretions
-
Ureterovesical junction competence
-
Urethral sphincter competence
-
Protective uroepithelial immune response (TLR4)
During the normal function of the urinary tract system, the body is able to protect and rid itself from invading bacteria. The bladder and urethra maintain a sterile environment by preventing bacteria from clinging to its structures. Bacteria are expelled out of the body during urination.
The normal composition of urine provides a bactericidal effect. Urine has a low pH and high osmolarity which most organisms cannot survive in. Urine also contains uromodulin and uroepithelium mucous secretions which act against bacteria.
In women, mucous production in the urethra traps bacteria before it can enter into the bladder.
Men have a longer urethra compared to women, making it harder for bacteria to enter the bladder. Men also produce mucous secretions from the prostate to protect them against infection.
The body’s immune response plays a key role in the fight against urinary tract infections. Immune response to bacteria begins once the bacteria passes the distal urethra and goes into the bladder. Toll-like receptors on the uroepithelium recognize bacterial patterns and initiate an immune response. This recruits neutrophils and macrophages which leads to phagocytosis and inflammation. Both pathogenic virulence and defense mechanisms influence host susceptibility and UTI presence.
UTI occurs when there is a break or alteration in the host’s defense mechanisms and pathogens occupy host and reproduce.

Figure 4. Bladder (Medical Microbiology, 2017)
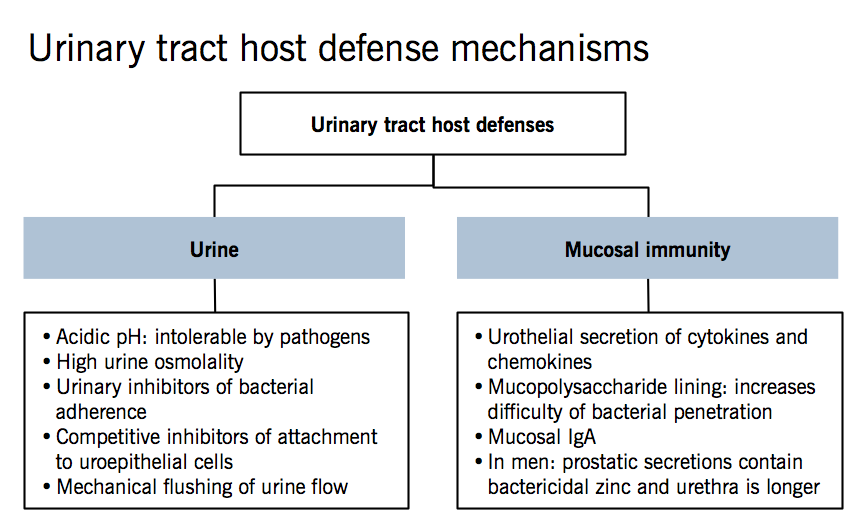
Figure 5. Urinary Tract Host Defenses Diagram (Wong, 2012).
RISK FACTORS FOR UTI INCLUDE:
- Premature newborns
- Prepubertal children
- Immunosuppressed
- Sexually active and pregnant women
- Diabetic
- Neurogenic bladder
- Urinary tract obstruction
- Antibiotic use that disrupts vaginal flora
- Spermicide users
- Estrogen-deficient postmenopausal women
- Individuals with indwelling catheters
ACUTE CYSTITIS PATHOPHYSIOLOGY – CORRECT DIAGNOSIS
- An infection can occur anywhere along the urinary tract including the urethra, bladder, ureter, or kidney.
- The most common type of UTI is acute cystitis.
- Acute cystitis is an inflammation to the bladder and is the most common site of UTI.
- Cystitis is a part of lower UTI, along with urethritis ( inflammation of urethra).
- Upper UTI include pyelonephritis (infection of upper urinary tracts – ureter, renal pelvis, and kidneys).
- Up to 50% of women may have a UTI at some point in their lives. Cystitis is more common in women because they have a shorter urethra than men, and that urethra is close to the anus.
- A gram-negative bacteria called Escherichia coli or E. coli accounts for the majority of UTI’s. E. coli will move from the gut into normally sterile urine, causing infection.
- E. coli is resistant to the urinary tract defense mechanisms. E. coli evades the immune response by producing toxins that kills complement cells. E. coli acquires its own nutrients through iron enabling it to grow fast. Patients with urinary catheters are especially susceptible to E. coli infections because they bind to latex and form a biofilm.
- Biofilms allow for increased colonization of bacteria and protection against host defenses and antibiotics. E. coli have flagella which allows them to move upstream during urination preventing expulsion. Pili allow E. coli to adhere to the uroepithelial wall and borough. This allows them to remain dormant until natural epithelial wall turns over (one month).
- Fungal infections are also responsible for causing UTI’s. They are usually uncommon but will affect immunocompromised individuals, one example is Candida.
CLINICAL MANIFESTATIONS:
- frequency
- urgency
- dysuria (painful urination)
- suprapubic (lower stomach/below umbilical region) pain
- low back pain
Caused by the body’s inflammation response to the pathogenic invasion.
Inflammation in the bladder wall stimulates stretch receptors leading to urgent and frequent urination.
Older adults with acute cystitis usually experience vague abdominal pain along with confusion.
It is important to keep in mind that UTI’s can be asymptomatic in some individuals.
Figure 6. UTI Card (Tumblr, 2019).
DIAGNOSIS:
According to McCance and Huether (2019),
- Urine cultures are used for UTI diagnosis.
- Cultures are measured for specific microorganisms. Urine must contain greater than 10,000/mL organisms for a patient to have a UTI.
- Antibiotic therapy should be used for treatment. The type of antibiotic will be based on bacterial sensitivity.
- A cystoscopy can be used to look at the bladder’s appearance in individuals with acute cystitis.
- In mild infections, the bladder’s mucosa will appear red. In more advanced infections, the mucosa will have hemorrhagic areas along with pus and exudates.
- If left untreated the infection can cause bladder wall necrosis.
Bladder inflammation – Acute Cystitis (hyperemic red – mild infection)

Figure 7. Cystitis (Smith, 2018).
More advanced type of acute cystitis – Hemorrhagic cystitis

Figure 8. Hemorrhagic Cystitis (American Urological Association, 2019)