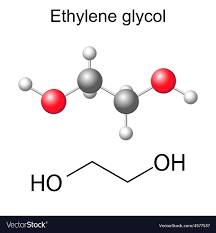
Left image: Chemical structure of ethylene glycol from: Accessed 20 June 2019.
Right image: Vial containing ethylene glycol from: Accessed 20 June 2019
Ethylene glycol is a liquid chemical that is colorless and odorless but does have a sweet taste. If ingested, this chemical is poisonous.
Sources
- Most commonly known as “antifreeze” (think of the stuff you spray on your windshield to get the frost off on a chilly winter day)
- Used as a coolant for car engines to keep from overheating in the summer
- Used as raw material in upholstery and fiberglass
- Found in household paints and detergents
This list is not exhaustive. Ethylene glycol has many uses and can be found in various products used every day. Please visit ChemicalSafetyFacts.org for more information regarding the above list and other possible uses.
*CONFUSION ALERT*
 Image from: Accessed 20 June 2019
Image from: Accessed 20 June 2019
Miralax and other like stool softeners go by the generic name Polyethylene glycol. These are drastically different compounds. The main difference in the chemistry is that ethylene glycol has a fixed, stable value and molecular weight whereas polyethylene glycol is NOT fixed and the molecular weight can change. For more detailed information and a great visual breakdown of the differences, please visit Pediaa.com
Biotransformation
Ethylene glycol is extremely water soluble. If ingested, it is quickly absorbed by the gastrointestinal tract. It can be absorbed through the skin and lungs, however this is a much slower process. Half life of ingested ethylene glycol is between 2 and 8 hours (depending on child versus adult). After only 24 hours, it is difficult to detect in the urine or body tissues, suggesting a very quick biotransformation.
Information derived from the Agency for Toxic Substances & Disease Registry. “Environmental Health and Medicine Education”. Accessed 20 June 2019.
Toxicokinetics and Mechanism of Action
Toxicity from dermal exposure or inhalation is unlikely.
Ingestion: When ethylene glycol is ingested, the liver metabolizes it. This can cause a feeling of intoxication, but the actual compound has a low toxicity. However, the liver uses several oxidation processes that break ethylene glycol down into different compounds that are more toxic than ethylene glycol:
- Ethylene glycol: Prior to oxidation – 2-8 hours after ingestion: Central nervous system affected characterized by dizziness, upset stomach, drowsiness, and/or seizures (1)
- Glycolaldehyde: First oxidation stage – 12-36 hours after ingestion: Metabolic process affected characterized by buildup of acid in body (metabolic acidosis), increased heart rate, jaundice, damage to mitochondria (1)
- Glycolic acid: Second oxidation stage – 24-72 hours after ingestion: Kidneys affected characterized by back pain and changes in urine output (2)
- Glyoxylic acid: Third oxidation stage – 36-72 hours after ingestion: Kidneys and tissues affected charaterized by renal trouble, dehydration, spasms (3)
- Oxalic acid: Fourth oxidation stage – within 72 hours after ingestion: Brain, heart, kidneys, and lungs affected characterized by organ failure and possibly death (4)
 (4)
(4)
Information derived from sources in order as they appear:
(1) Agency for Toxic Substances and Disease Registry. (2012) “Ethylene glycol and proylene glycol toxicity what is the biological fate of ethylene glycol?” Environmental Health and Medicine Education.
(2) PubChem. (2019). “Glycolic acid”. U.S. national Library of Medicine.
(3) Toxnet. (2013). “Glyoxylic acid”. Environmental Health & Toxicology.
(4) Eder, et al. (1998). “Ethylene glycol poisoning: toxicokinetic and analytical factors affecting laboratory diagnosis”. Clinical Chemistry. 44:1.
Target Organs and Signs/Symptoms of Toxicity
 Image from: Accessed 20 June 2019
Image from: Accessed 20 June 2019
This visual is a good depiction of the information described above. Different products of the ethylene glycol oxidation process target different organs.
- CNS – mirrors alcohol intoxication: nausea, convulsions, coma
- Kidneys – kidney failure, metabolic acidosis
- Liver – yellowing of skin and sclera (whites of eyes)
- Overall organ system failure – severe bodily shock, death
Only about 4 ounces of ethylene glycol is needed to cause death in an average-sized male
Treatment
Tests:
- Arterial blood gas analysis
- Liver function panel
- Complete blood count / Ethylene glycol blood test
- Urinalysis
- Test for bodily functions such as CT scan, EKG, chest x-ray
Medical treatments:
- Activated charcoal
- Intravenous sodium bicarbonate (for acidosis)
- Fomepizole (antidote)
Information for signs/symptoms/treatment derived from: MedlinePlus. “Ethylene glycol poisoning”. Accessed 20 June 2019.
Biomarkers
- Blood gasses
- Urinalysis
- Serum calcium concentration (newer biomarker)
This abstract from an article published in 2017 by Hodgman, Marraffa, Wojcik, & Grant shows why newer biomarkers are necessary for ethylene glycol poisoning.
“Abstract
The diagnosis of ethylene glycol intoxication can be challenging. Definitive testing for ethylene glycol is not readily available and clinical decisions are often based on clinical suspicion and the results of more readily available tests. One of these findings is hypocalcemia, presumable through complexation with the ethylene glycol metabolite oxalate.”
Unique Exposure
There are no readily available cases of unique exposure to ethylene glycol, however there are many incidents of its use in suicide attempts and accidental ingestion by children and pets. The CDC has provided a list of trade names for ethylene glycol. While ethylene glycol is naturally a clear substance, neon colors are typically added to it to identify it as antifreeze.