Differential Diagnosis I:
Pneumonia
Rationale:
Pneumonia is the infection and inflammation of the terminal airways and alveoli. The most common agents that cause pneumonia are viruses followed by bacteria and atypical microorganisms, such as fungi (McCance & Huether, 2019, p. 1186). Mr. Smith has many of the typical signs and symptoms of pneumonia. He reports shortness of breath and sharp chest pain. He also presents with tachypnea, circumoral cyanosis, and decreased oxygen saturations. With an extensive smoking history and being in his sixties, Mr. Smith is at an elevated risk of developing pneumonia. These risk factors, combined with his abnormal vital signs (respiratory rate and oxygen saturations), patient reports of SOB and chest pain, provide a rationale for considering pneumonia as a differential diagnosis.
In the diagnosis of pneumonia, a chest X-ray would typically reveal infiltrates, and the white blood cell count would usually be elevated (McCance & Huether, 2019, p. 1186). However, upon reviewing Mr. Smith’s chest X-ray, no infiltrates were noted, and his white blood cell count was within a normal range. Thus one can exclude pneumonia as the official diagnosis.

Figure 1. Chest X-ray showing Pneumonia (Bujara, 2019).
Differential Diagnosis II
Acute Exacerbation of Congestive Heart Failure
Rationale:
Congestive Heart Failure (CHF) develops when the heart becomes unable to pump blood effectively to meet the body’s metabolic demands. Perfusion to the kidneys decreases, causing the renal system to activate the RAAS system and resulting in fluid retention and increasing the preload and afterload of the heart. Over time, the heart muscles stiffen and their ability to contract weakens, and fluid and blood starts to back up in the lungs and other parts of the body. In an acute exacerbation of congestive heart failure, patients often have signs and symptoms related to respiratory distress, such as shortness of breath, tachypnea, cyanosis, and decreased oxygen saturations, and they can present with chest pain and swelling of the legs and feet (McCance & Huether, 2019, p. 1098-1101). Patients like Mr. Smith, who has a history of hypertension and tobacco usage are at an elevated risk for developing CHF. Taking all of these factors into consideration, CHF is an obvious differential diagnosis for a pulmonary embolism. (McCance & Huether, 2019)
However, in acute exacerbation of CHF, bilateral peripheral edema will be observed along with fluid build up in the lungs (accompanied by abnormal breath sounds such as crackles). Patients with CHF exacerbation typically experience sudden weight gain as a result of fluid retention, and their BNP levels are extremely elevated. Mr. Smith presents with unilateral lower extremity edema, diminished lung sounds without crackles, and a stable weight. His BNP levels, while slightly elevated, are not high enough to be considered a sign of heart failure. In addition, patients with an acute exacerbation of CHF can often present with lower sodium levels due to being in fluid overload as well as an enlarged heart. Mr. Smith’s sodium levels were within normal limits, and his chest X-ray did not show cardiomegaly. Considering all of these findings, it is safe to determine that Mr. Smith’s diagnosis is not an acute exacerbation of congestive heart failure.

Differential Diagnosis III
Tension Pneumothorax
Rationale:
Pneumothorax is the presence of air or gas in the pleural space, usually as a result of a rupture in the visceral pleura or the parietal pleura and chest wall. During inspiration, air accumulates in the pleural space, separating the visceral and parietal pleura. This creates a disturbance in the negative pressure of the pleural space and inhibits the ability of the lung(s) to expand, causing the lung(s) to collapse inward. As a result, the lung’s ability to participate in gas exchange is impaired. In a tension pneumothorax, there is a one-way valve that allows air to get in but not out, allowing for even more air accumulation to occur. This is considered a medical emergency (McCance & Huether, 2019, p. 1168). Mr. Smith exhibits many of the classic signs and symptoms of a tension pneumothorax such as sharp chest pains, shortness of breath, tachypnea, circumoral cyanosis, light-headedness, and decreased oxygen saturations. In addition, Mr. Smith’s smoking history puts him at a greater risk of developing a pneumothorax, thus makes pneumothorax an appropriate differential diagnosis.
However, Mr. Smith’s chest X-ray did not show any air in the pleural cavity; thus one can eliminate pneumothorax as the official diagnosis.

Figure 3. Chest X-ray of Right Pneumothorax (University of Virginia, 2013).
Differential Diagnosis IV
Myocardial Infarction
Rationale:
Myocardial infarction, the medical term for heart attack, occurs when there is a prolonged occlusion to blood flow to the coronary arteries, resulting in irreversible myocardial death (McCance & Huether, 2019, p. 1083). Individuals experiencing a heart attack typically present with severe chest pain and shortness of breath with decreased oxygen saturations and, in some cases, cyanosis. Patients like Mr. Smith with a history of hypertension and smoking are at an elevated risk for the development of myocardial infarction due to the damage that occurs to the blood vessels as a result of high blood pressure and tobacco exposure. Mr. Smith presents with many of the classic symptoms of a heart attack such as dyspnea, tachycardia, sharp chest pain, low oxygen saturations, and being light-headed. Combined with his uncontrolled hypertension and his extensive smoking history, Mr. Smith could easily be diagnosed with a myocardial infarction.
However, Mr. Smith’s EKG came back as sinus tachycardia with no other abnormal findings (such as ST elevation or ST depression), and his troponin levels were normal. In a heart attack, there would be additional changes in the EKG besides heart rate, and the troponin levels would be high as myocytes begin to die (McCance & Huether, 2019, p. 1086). Thus one can eliminate MI as the final diagnosis for Mr. Smith.
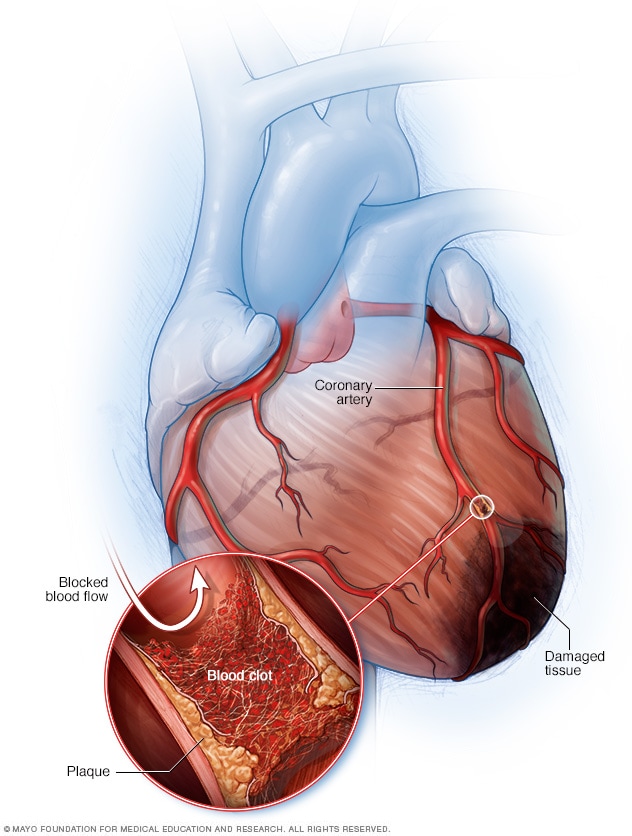
Figure 4. Heart Attack. (Mayo Clinic, 2018)