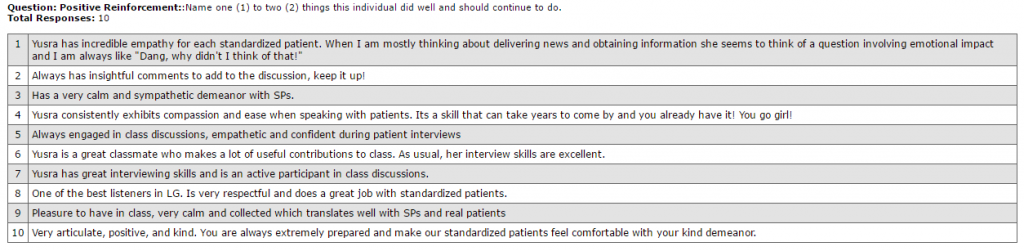
“Yusra is functioning at a level that is above most of her peers” an attending wrote about me at the end of my ambulatory general medicine rotation. He further wrote “She is on her own developing a good differential and explaining what she believes to be the most prudent next step which is often correct. I am very impressed with her.” Starting third year, I wasn’t too worried about interacting with patients. I had felt comfortable doing this during standardized patient interactions in my first two years of medical school and had often heard from my peers that I “consistently exhibit[s] compassion and ease when speaking with patients.” I was more concerned about developing and prioritizing a differential diagnosis for my patients’ chief complaints and presenting accurate history and supporting evidence for my differential diagnosis . I understood that clinical medicine has two key components: patient interaction and clinical reasoning. When my ambulatory attending, during the third month of my third year, wrote that I was presenting patients’ histories in a concise manner and developing good differentials, I was encouraged that I was on the right track. I wanted to continue practicing and mastering these skills during the remainder of my third year. Furthermore, his comment that I was often accurate in presenting the most prudent next step in patient management encouraged me to continue challenging myself in this regard and continue presenting management plan for my patients.
Arriving at a final diagnosis and developing a management plan was often challenging on sub-specialty services as patients presented with complex medical conditions. However, I learned through experience that if I use clinical evidence to develop and prioritize my differential diagnosis in a problem focused format, this will automatically lead me to a management plan. I used this strategy during my hepatology rotation at the end of my third year when the cause of renal failure in the setting of hepatic failure was not always clear. In the last week of my rotation, I presented an overnight admission who I considered to be in type two hepatorenal syndrome given her creatinine and urine chemistry trend, with acute anemia from a suspected variceal blead and tense ascites due to diuretic non-compliance worsening her pre-renal acute kidney injury. I proposed that instead of performing paracentesis, we continue to infuse her with albumin and conduct endoscopy to control any source of bleeding. I thought paracentesis would worsen intravascular volume depletion and acute kidney injury while an active bleed was suspected. I was controlling the quivers of my voice while I presented this case because I was intimidated by its complexity. To my excitement, my attending physician agreed with summary of the clinical picture and management plan. Furthermore, I proposed that the patient should be sent home with home health since she was non-compliant with medications; ensuring diuretic compliance was essential to prevent another hospitalization. I sensed the smile on my attending’s face when I proposed this plan since last week he had coached me to be farsighted in anticipating patients’ medical in developing discharge plan. I could integrate his teaching in developing my patient’s management plan.
At the end of my rotation, my hepatology attending wrote that I “performed at the level of a mid-year PGY1.” I could achieve such excellence in patient care because of my desire to constantly challenge myself and integrate in my practice any feedback I received from my seniors. I am encouraged that I have built strong roots in patient care skills during medical school that I can further build upon during residency. Ophthalmology, being a specialized surgical field, will expose me to clinical knowledge and instruments I have never learned before. It will be important for me to continue to challenge myself in areas of clinical knowledge and patient care and look up to my attending physicians and senior residents for guidance. Through self-determination, constant practice, and setting my eyes at the goal i.e. to become a competent ophthalmologist, I will be able to perform well during residency and master the skills of patient care as they pertain to ophthalmology.