Before medical school I ran middle-distance events as part of my college track and field team. While largely thought of as an individual sport, it takes a team effort to win track meets. This was exemplified during my junior year when my team unexpectedly won the conference championship. We were not picked as favorites that year but little by little points scored across the team added up. Everyone’s individual efforts mattered, and with scorers from all facets of our team we were able to take home the trophy. I see a lot of parallels to be drawn with regards the team-based approach to patient care within our health care system. Rarely anymore is one physician making all the calls in the hospital, rather the case is discussed in detail every morning by a multi-professional rounding team. Even on the outpatient side the goal is to connect patients into a “medical home,” with different offices and practices working together. Everyone plays an important role and functioning as a team is required for successful patient care.
- A few of my college track teammates
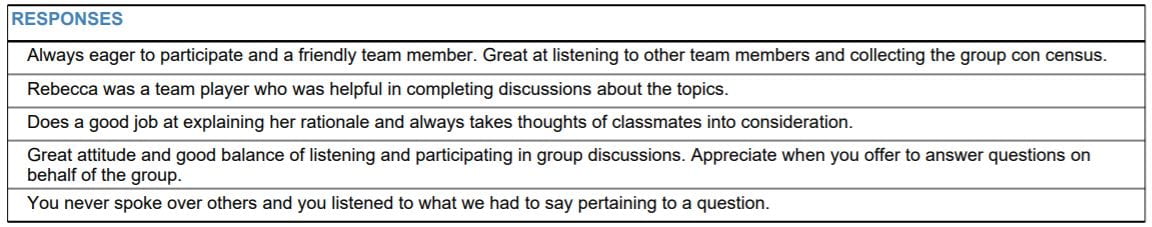
- The wonderful Gen Med 8 Team
During my third-year clerkships I’ve been fortunate to have worked on many excellent healthcare teams. One particular standout is the month I spent on a general medicine inpatient service; never before had I been part of a team that worked so efficiently together. I came home every day energized and excited by how much I had learned, how we had helped a patient that day, and how much fun I had had! I took special care to note what specifically made this a wonderful experience:
- Everyone did their job well. The anesthesia intern was one of the most efficient residents I had ever met. This therefore enabled our senior resident to spend time on teaching, leading the team, and checking in with the medical students on pre-rounding. The attending was a fantastic listener and offered teaching points on patient care plans in a way that was supportive and educational.
- Communication on the team was strong. In sharing a team room with the case manager we were able to check in early and often about discharge needs for patients. We spoke with pharmacy daily either via phone or in person. We had a system for contacting nursing staff to round with us every day. Our senior resident had prepared a “face sheet” so when we walked into patient rooms they knew who we were and what our roles on the team were. Discussions about patient care decisions were supportive and collaborative, I was never afraid to ask questions.
- Expectations were laid out early and clearly. It helped me immensely to know what my role on the team was, how learning would be taking place, and when to expect feedback. I was encouraged to come up with goals for the month which were then written and hung on the wall of the team room for accountability and frequent progress checks. Everyone was on the same page, which helped everyone fulfill their role successfully.
This teamwork not only benefited my teaching, it allowed us to provide a superior hospital experience for our patients. Our collective efficiency allowed us to spend more time in patient rooms discussing the care plans, and if patients ever had any questions each team member was equally prepared to answer. The positive, supportive energy of our team gave us the capacity to be more empathetic towards patient concerns. We had a difficult case that month where a woman on our service wanted to leave AMA. Our team went to speak to her, and over the course of discussing why it was important to stay in the hospital the conversation kept coming back to the patient’s desire to go home and drink a Mountain Dew. We tried to explain her disease process, and to impress our worries for her safety, but again the patient responses all circled around not being able to get a Mountain Dew. I think it would have been very easy to continue to try and force our agenda here had team members been more stressed or burnt out, but it became apparent that it was less about a Mountain Dew and more that the patient felt that she wasn’t being respected in the hospital and people weren’t listening to her. We regrouped and acquired (almost magically, given hospital cafeteria rules) a Mountain Dew from one of my classmates’ medical school lockers; by bringing the patient the Mountain Dew she was immediately appreciative, trusted our team more, and was ready to discuss her treatment plan. Through this small gesture we were able to meet the patient where she was, so-to-speak, and give her back a component of dignity and humanity she felt she had been denied prior to this. She ultimately went on to get all the necessary tests and was able to be safely discharged shortly thereafter.
On the other hand, I’ve sadly also seen how poor team dynamics can negatively affect patient care. On a different general medicine service later in the school year I was part of a team where the senior resident and attending physician openly did not get along. I felt somewhat lost in my role because expectations held for me by my senior resident differed slightly from those of the attending. Team communication felt more strained, and team members on all levels seemed more stressed. While I still feel we were able to provide safe and effective care for patients, I don’t think it was quite at the level of empathy and patient-centeredness as my other gen med experience. We had a patient during this time who had been admitted for treatment of a severely infected wound as a result of injection drug use. While initially she was very worried about her condition, she became very irritable as symptoms of withdrawal set in during the afternoon and she ultimately AMA. As a team we had offered treatment for withdrawal symptoms and resources for social concerns, but we couldn’t convince her to stay for treatment. After she left I couldn’t help compare her case to the patient who had wanted a Mountain Dew; I felt like we didn’t do as good of a job of meeting the patient where she was in this case, and I think a major reason for this was the added strain on our team from poor team dynamics. Team members including our senior resident were more burnt out and less able to give patients the empathy and patience required to care for them.
In graduating from medical school and going into residency next year I will be playing a new role within the healthcare system, filling a new spot on the healthcare team. In order to help my team the best, I will need to not only do my job well but keep an eye on overall team dynamics, and feel empowered to make changes if team dynamics are limiting the potential of the team. Part of doing my job well will involve keeping up to date on my medical knowledge, learning to be efficient with documentation and the electronic medical record overall. I plan to further refine these skills during the end of my M4 year through my sub-I month on a cardiology service, and a hospital medicine elective where I will work directly with an attending to practice efficiently carrying a team of patients entirely on my own. I will work on anticipating questions or problems ahead of time regarding medications or discharge plans for my patients so I can communicate effectively with other members of the care team, including pharmacists, case managers, and nursing staff, to resolve those problems early. And finally, I will check in with and watch out for other members of my team, because after all that’s the greatest benefit of being on a team: whether you’re having a bad race or a difficult day at the hospital, teammates are there to boost you back up when you need it. Teammates are what make the early morning track workouts and long days at the hospital worth it; teammates ultimately help us achieve new PR’s and conference championships as well as deliver the highest form of patient-centered care.