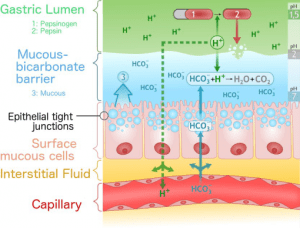
Normal physiology of the peptic tissues and mechanisms
The peptic tissue includes two major layers (mucous barrier & surface mucous cells) and utilizes numerous gastric mucosal mechanisms to safely contain the digestive gastric acid.
- Epithelial cells
- secrete a protective, gel-like mucus layer to protects gastric mucosa against autodigestion from pepsin and erosion by acids and other caustic materials from ingestion.
- secrete bicarbonate ions to neutralize acids from the lumen
- form tight junctions to repel harsh fluid that may injure the stomach lining
- Mucosal blood flow
- retrieves excess hydrogen ions back-diffused into the mucosa from the lumen and transport bicarbonate to mucosa
- sustains high cellular metabolic and regenerative activity
- Mucosal prostaglandins
- promotes secretion of bicarbonate
- promote production of gel mucous barrier
- maintain mucosal blood flow (vasodilator)
Figure 1. Cross section of peptic tissue (Glyn, 2018)
Pathophysiology
Breakage or ulceration of the protective mucosal lining in the lower esophagus, stomach (i.e., gastric ulcers), and duodenum (i.e., duodenal ulcers; most common).
Figure 2. (A) Endoscopic and (B) histologic cross section views of peptic ulcer (Pathology for health Professionals 4th. edition, 2013)
Underlying causes
- Inhibition of prostaglandin synthesis by aspirin and NSAIDs — decrease in protective mucus production, decrease in bicarbonate secretion (decrease in buffering capacity).
- Causative agents allow acid and pepsin to penetrate the mucosal barrier, leading to ulceration, e.g., Helicobacter pylori. H. pylori produces urease which assist in creating alkaline microenvironment to survive the low acidic gastric environment. The pathogen cause inflammation and disrupt mucosal defense and regeneration, resulting in chronic ulceration.Habitual use of aspirin/NSAIDs, H. pylori, alcohol, bile salts, acid, and pepsin weakens the mucosal barrier and allows a greater extent of hydrogen ions back-diffuse to epithelial cells — causing injuries to epithelial cells, disrupting permeability and cellular function, and loosening the epithelial junctions.
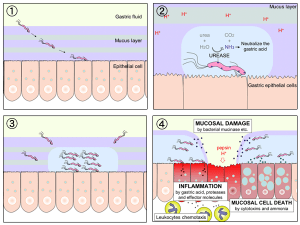
Figure 3. Helicobacter pylori produces ureas that could create a more alkaline microenvironment for it to survive (Khan, Karim & Iqbal 2009) - Stress-Related factors secondary to serious illness or ischemic conditions, such as multiple system organ failure, head trauma, and severe burn, resulting in multiple ulceration or ischemia in the stomach and/or duodenum.
Risk factors
H. pylori, habitual use of aspirin and/or NSAIDs, alcohol, smoking, chronic obstructive pulmonary disease, and acute pancreatitis.
Key criteria for diagnosis
- Epigastric pain – burning sensation occurs after meals (gastric ulcers), 2-3 hours after meal or in the middle of night (duodenal ulcers) due to sensorineural stimulation by acid or muscle spasm. Duodenal pain could be immediately relieved by ingestion of food or NSAIDs.
- Habitual use of aspirin and/or NSAIDs.
- Presence of pylori.
- Bleeding — more often seen in stress-related mucosal diseases with coagulopathy or mechanical ventilation.