Myocardial Infarction
A myocardial infarction is a pathological condition in which a portion of the heart experiences ischemia. Upon the onset of ischemia, ECG changes can be seen within 30-60 seconds. However, the death of cardiac cells won’t occur until 20 minutes of sustained ischemia has taken place. Once cardiac cells have died, necrosis occurs within the area of ischemia and the damage is irreversible. The damage can lead to dysfunction of the heart and increased workload. Ultimately, a myocardial infarction can lead to death if enough of the myocardial tissue becomes ischemic and necrotic (McCance & Huether, 2019, p. 1083-1085). The symptoms of a myocardial infarction include the following: intense, crushing chest pain; shortness of breath; epigastric pain; nausea and vomiting; heart palpitations; immense fatigue; upper-back pain; and pain that radiates down the left arm (Ro, Lang, & Warp, 2004). Some clinical manifestations of a myocardial infarction include an elevated ST segment on the ECG (STEMI myocardial infarction), elevated cardiac troponin 1 levels, and dysrhythmias (McCance & Huether, 2019, p. 1086-1087). Our patient presented with chest pain as well as epigastric pain and nausea. Upon the completion of a set of tests including a blood panel and ECG, it was found she had an elevated ST segment and increased troponin levels. An MI was ruled out as a result of a normal echocardiogram that demonstrated no ischemia.
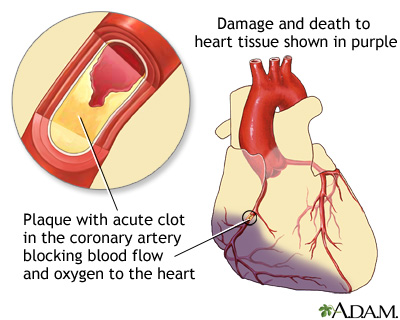
(Heart attack: medlineplus medical encyclopedia, n.d.)
(Coronary artery disease – STEMI topic review, n.d.)
Peptic Ulcer
A peptic ulcer is an abnormal opening in the mucosal lining of the gastrointestinal tract. These ulcers can occur in the lower esophagus, stomach, or duodenum, and they can range from a small, singular ulcer to multiple, large ulcers. Individuals may have chronic or acute peptic ulcers, and the severity of the damage can range from superficial to deep. If an ulcer permeates the entire mucosa and injures the blood vessels, then it is considered a true ulcer. True ulcers can cause serious damage to the body including hemorrhage and gastric wall perforation (McCance & Huether, 2019, p. 1332). Symptoms of peptic ulcers include the following: epigastric abdominal pain; postprandial fullness/pain; nausea and vomiting; anemia; dysphagia; unexplained weight-loss; and odynophagia (Gheonea et al., 2009; Narayanan, Reddy, & Marsicano, 2018). Some clinical manifestations of peptic ulcers include gastric bleeding, a positive urea breath test, and the presence of H. pylori bacteria (Narayanan, Reddy, & Marsicano, 2018; McCance & Huether, 2019, p. 1332-1333). Our patient presented to the ER with abdominal pain, nausea, and increased pain after eating a large meal. A peptic ulcer was ruled out due to a negative urea breath test and a negative H. Pylori blood antibody test.
.jpg)
(Smith, 2019)
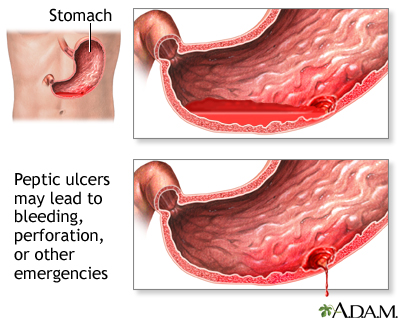
(Peptic ulcer: medlineplus medical encyclopedia, n.d.)
Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is a gastrointestinal condition that is the result of abnormal brain-gut interaction. IBS does not have a known pathophysiology with regards to structural or biochemical reactions, however research has shown promise in the disease being a dysfunction of multi-system interactions. Some of conditions often associated with IBS include hyperalgesia, food intolerances/allergies, and psychosocial issues such as immense stress or abuse (McCance & Huether, 2019, p. 1339-1340). The symptoms of IBS include the following: constipation; diarrhea; abdominal pain/discomfort; feeling of urgency when needing the defecate; mucous covered stools; postprandial worsening of pain; and bloating (McCance & Huether, 2019, p. 1340; Enck et al., 2016). Some clinical manifestations of IBS include the symptoms being chronic (at least one day per week for at least three months) and exclusion of other conditions such as Crohn disease or diverticulitis (McCance & Huether, 2019, p. 1340). The exclusion of other gastrointestinal diseases may include procedures such as colonoscopy or endoscopy, C-reactive protein marker blood tests, and food allergy testing (McCance & Huether, 2019, p. 1340). Our patient presented with abdominal pain and postprandial worsening of the discomfort. She denied history of abnormal stools or abdominal cramping, and this enabled IBS to be ruled out.

(Integris, n.d.)
:max_bytes(150000):strip_icc()/ibs-pain-locations-1945305-5c04ab7ec9e77c0001dbe853.png)
(Bolen, 2019)