Ulcerative Colitis
Rationale: Ulcerative colitis (UC) is a chronic inflammatory disease that causes ulceration of the colonic mucosa, most commonly in the rectum and sigmoid colon (McCance & Huether, 2019). Symptoms of UC can be very similar to Crohn’s disease (CD) which makes them challenging to differentiate from each other. Similar symptoms between the two include large amounts of diarrhea, cramping pain, urge to defecate, and mouth ulcers (involved with extraintestinal manifestations). The patient, Svetlana, experienced painful diarrhea with extreme urgency and ulcerations in the mouth. She also complained of fatigue and had inelastic skin turgor which could be a result of anemia or dehydration, both of which are symptoms of severe UC. Additionally, the age of onset for both diseases is between 10 and 30 or 40 years, which is where the patient falls at 16 years old.
However, where UC differs from CD is in the location of the disease and the pathophysiology. UC involves the rectum and may extend proximally to the colon, where CD affects any part of the gastrointestinal tract from the mouth to anus (McCance & Huether, 2019). Additionally, CD involves skip lesions that spread with transmural involvement, whereas UC does not involve skip lesions and is not transmural. In Svetlana, her scope showed skip lesions throughout her intestines with the worst of it found in her terminal ileum (intestines). It also showed transmural inflammation with cobblestone mucosa, which is characteristic of CD. Due to these results, UC can be ruled out as the diagnosis.
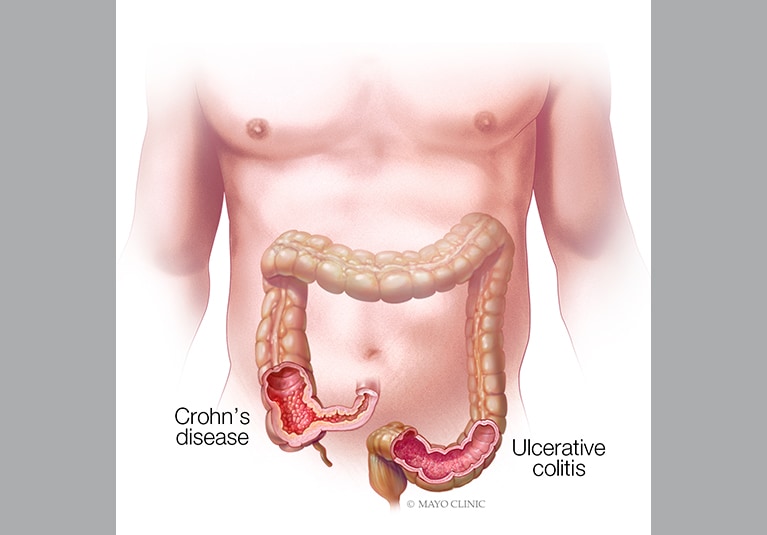
Ulcerative colitis compared to Crohn’s disease (Mayo Clinic, 2019)
Irritable Bowel Syndrome
Rationale: Inflammatory bowel syndrome (IBS) is considered a disorder of brain-gut interaction characterized by abdominal pain with altered bowel habits (McCance & Huether, 2019). Some similar symptoms between IBS and CD include lower abdominal pain and fecal urgency. IBS is more common in women, especially in youth and middle age which is similar to risk factors of CD of being less than 40 years and having a slight predominance for women. Being a female of 16 years old, these factors are relevant to Svetlana’s diagnosis. Svetlana complained of fatigue and had observational malnutrition and nutrient deficiencies. With depression and anxiety being common in individuals with IBS, associated symptoms such as loss of appetite and sleep disturbances could be contributing to her fatigue and malnutrition.
However, where IBS differs from CD is in the diagnosis and relief of symptoms. There are several characteristics that factor in diagnosing an individual with IBS. There are also limited diagnostic tests needed in the absence of “alarm symptoms,” such as fever or an abdominal mass when diagnosing those with IBS (McCance & Huether, 2019). With Svetlana’s chief complaints and assessment results, her disease would be better characterized as CD. Additionally, individuals with IBS usually experience relief after defecation, while Svetlana’s pain did not improve with bowel movements. Due to these reasons, IBS can be ruled out as the diagnosis.

Pathophysiology of irritable bowel syndrome (O’Hara, 2019)
Appendicitis
Rationale: Appendicitis is an inflammation of the vermiform appendix, which is a projection from the apex of the cecum (McCance & Huether, 2019). Some similar symptoms between appendicitis and CD include right lower quadrant (RLQ) pain and diarrhea, which could possibly occur in those with appendicitis. Lab results for both diseases also show elevated white blood cell (WBC) counts. Svetlana complained of RLQ pain and diarrhea, as well as had elevated WBC in her lab results. The age of onset for appendicitis is between 10 and 10 years, similar to CD at 10 to 30 years, which is where Svetlana falls at 16 years old. Additionally, anorexia commonly follows the onset of pain in patients with appendicitis which could be a contributing factor to Svetlana’s malnutrition and/or amenorrhea.
However, where appendicitis and CD differ are in the location of pain and the pathophysiology. While appendicitis does involve RLQ similar to CD, epigastric and periumbilical pain are also typical symptoms associated with an inflamed appendix. Svetlana did not report any pain other than in her RLQ which would help rule out appendicitis. Additionally, appendicitis is thought to be caused by an obstruction of the lumen, either due to stool, tumors, or foreign bodies, which was not observed in Svetlana’s assessment. CD, on the other hand, is most likely thought to be due to a genetic mutation of CARD15/NOD2 (McCance & Huether, 2019). Due to these reasons, appendicitis can be ruled out as the diagnosis.
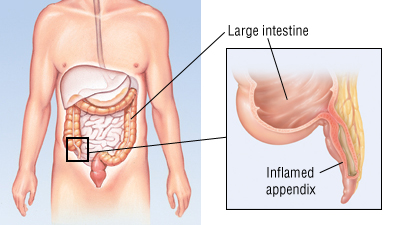
Inflammation of the appendix (Harvard Health Publishing, 2019)