Normal Physiology: Pericardial Sac
The pericardium is a protective layer that covers the outside of the heart and greater vessels. It is described as a “double-walled membranous sac (McCance, 2019)” that serves several functions of the heart. It protects the heart from infection due to its close proximity to the lungs and pleural space, it prevents drastic movement of the heart, and contains pain receptors, as well as mechanoreceptors that detect changes in blood pressure and heart rate. The structure of the pericardium itself is comprised of two layers: the parietal and visceral layers. In between, is a fluid filled gap known as the pericardial cavity. Cells in the mesothelial layer of the pericardium secrete 25-30 ml of pericardial fluid that aids in prevention of rubbing and irritation by surrounding structures (McCance, 2019).
Pathophysiology: Acute Pericarditis
Description: Acute pericarditis is a common disorder of the pericardium that involves inflammation of the pericardium that can also present with or without pericardial effusion. In the incidence of infection, this area becomes inflamed and produces an abnormal amount of fluid leading to complications (Imazio, 2011). Acute pericarditis is a fairly new condition being studied and has several different incidences including: infections, autoimmune, trauma, drug-related and most often is idiopathic. Viral pericarditis (Epstein-Barr, hepatitis, HIV, measles, mumps, varicella, influenza) is the most common etiologic agent (Imazio, 2011). Tuberculosis is another common bacterial cause for this condition.

(Admin, 2015).
Manifestations:
- fever
- malaise
- sudden onset of chest pain (retrosternal)
- shortness of breath
- dyspnea
Diagnosis: To confirm the condition of pericarditis, usually two out of four of the following manifestations must be present: chest pain, friction rub, widespread ST segment elevation, and pericardial effusion (Imazio, 2011). Other diagnostic tools are useful in confirming acute pericarditis such as echocardiogram, chest X-ray, auscultation, and lab inflammatory markers.
ECG signs: Upward concave ST-segment elevation, PR segment depression, Spodick’s sign (down sloping of TP segment).
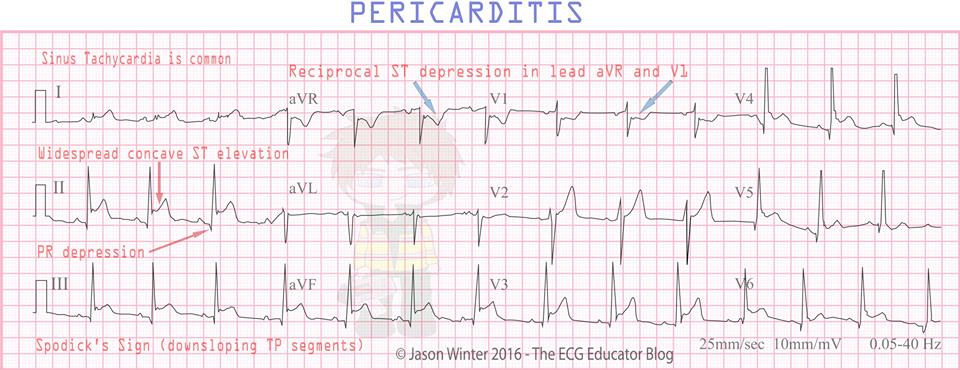
(Winter, 2016).
Labs: Inflammatory markers (c-reactive protein, creatine kinase, troponin).
Treatment: NSAIDs are first line treatment.
- Anti-inflammatory medications.
- Aspirin
- Ibuprofen
- Corticosteroids
- Colchicine: antigout med that acts as an anti-inflammatory agent (prevents fibrosis)
- Pericardiectomy (recommended for persistent constrictive pericarditis)
Complications: Major complication includes cardiac tamponade, corticosteroid dependence, constrictive pericarditis, recurrent pericarditis. The most serious of these complications is cardiac tamponade, which most often presents with dyspnea, tachycardia, jugular vein distention, cardiomegaly, and pulsus paradoxus (McCance, 2019). Constrictive pericarditis is a condition that is characterized by fibrous scarring of the pericardial cavity. This further limits the heart in its ability to relax and contract, causing a cascade of of issues (much like cardiac tamponade) such as: reduced ventricular filling, impaired ventricular relaxation, and reduction in cardiac output (McCance, 2019).

(Mona, 2015).