Meningitis
Normal Physiology
The brain and spinal cord are surrounded by protective membranes known collectively as the meninges. As seen in Figure 1, the meninges are made up of three membranes, the dura mater, the arachnoid mater, and the pia mater. The outermost membrane, the dura mater, which translates to “hard mother”, is the thickest and toughest of the meningeal layers. The arachnoid mater, a web-like membrane, lies beneath the dura mater with the subdural space running between the two membranes. Beneath the arachnoid mater lies the pia mater. This delicate membrane is the closest to the brain and spinal cord and provides support for the vasculature that supplies blood to the brain tissue. The space between the pia mater and the arachnoid mater is the subarachnoid space. This space contains cerebrospinal fluid . The primary function of this fluid is to cushion and protect the brain and spinal cord, however it also removes waste from circulation in the CNS .
Figure 1. The Meningeal Layers (Pearson Education, Inc, 2011)
Figure 1 retrieved from https://www.studyblue.com/notes/note/n/chapter-15/deck/5754539
Pathophysiology
Meningitis is a disease process where the protective layers that cover the brain and spinal cord become inflamed. Meningitis can be infectious or it can be caused by injury, cancer, and other noninfectious causes. Infectious meningitis can be caused by a bacterial, viral, or fungal infection. It can also be caused by parasites or other toxins. Diagnosis of meningitis is dependent upon a physical examination, blood cultures, nose and throat swab, and CSF analysis and cultures (McCance & Heuther, 2019).
Bacterial Meningitis
Bacterial Meningitis is a life-threatening infection most often caused by the pathogens Meningococcus (Neisseria meningitidis) and Pneumococcus (Streptococcus pneumoniae). Infections occur primarily in adolescents and children under the age of one. The infection is spread through contaminated saliva, respiratory tract secretions and respiratory droplets. Infection occurs when these pathogens are inhaled. As can be seen in Figure 2, the bacteria will then attach to the epithelial cells in the nasopharynx, cross the mucosal barrier and enter the blood stream. After the bacteria enters the blood stream it will travel to the cerebral blood vessels where it will cross the blood brain barrier and infect the meninges. After the bacteria crosses the blood brain barrier it will multiply rapidly and lyse in the subarachnoid space releasing bacterial endotoxins. This rapid multiplication will attract a large number neutrophils to the area where they will release inflammatory cytokines to fight the infection. This release of endotoxins and cytokines increases the permeability of the blood brain barrier causing cerebral edema and brain tissue damage. The exudate from the inflammatory response will also thicken the CSF, obstructing flow around the brain and spinal cord. This paired with edema will increase the intracranial pressure which if not corrected will lead to cerebral ischemia, necrosis and subsequent cerebral infarction (McCance & Heuther, 2019).
Figure 2. The Pathogenesis and Pathophysiology of Bacterial Meningitis (Tunkel & Scheld, 1993)
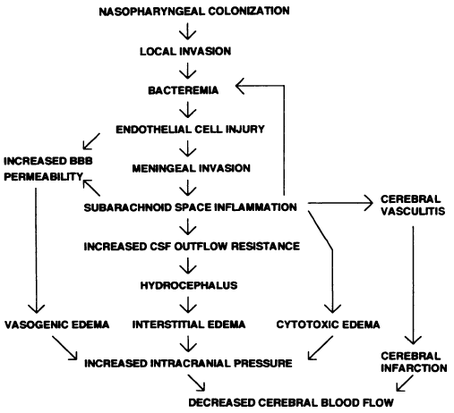
Figure 2 retrieved from https://www.semanticscholar.org/paper/Pathogenesis-and-pathophysiology-of-bacterial-Tunkel-Scheld/f40c0485d64f6a3ccb19c4a790d12bb392f73372
Viral Meningitis (Aseptic Meningitis)
Viral Meningitis is the most common form of meningitis in the United States. The symptoms are typically more mild that bacterial meningitis and often the infection will resolve without treatment. In viral meningitis the infection is limited to the meninges, and the CSF will not have an identifiable pathogen. The virus that causes the infection enters the brain through infected leukocytes and will then infect the vascular endothelial cells. The pathogens then enter the subarachnoid space, the subsequent immune response will lead to inflammation and increased permeability of the blood brain barrier which allows more circulating immunoglobulins can enter the CNS to combat the infection (McCance & Heuther, 2019).
Fungal Meningitis
Fungal meningitis is a rare form of meningitis that is caused by the inhalation of fungal spores, see Figure 3. Fungal meningitis is not communicable from person to person. The infection causes a chronic disease process that can develop gradually but with harmful effects. The fungal infection in the central nervous system can produce a granulomatous reaction which causes the formation of granuloma or gelatinous masses that often will develop in the meninges at the base of the brain. The infection can spread from the meninges into the brain tissue resulting in thrombosis, infarction and communicating hydrocephalus. Fungal meningitis most often affects immunocompromised individuals (McCance & Heuther, 2019).
Figure 3. Route of Infection of Cryptococcal Meningitis (Xue C., 2012).
Figure 3 retrieved from https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1002869
Clinical Presentation
The clinical manifestations of a patient with meningitis will differ in intensity and presentation depending on the type of microorganism causing the infection. These clinical manifestations can be grouped into three categories, infectious signs, signs of meningeal inflammation, and neurological signs. The clinical signs of meningeal irritation include a throbbing headache, photophobia, nuchal rigidity, and positive Brudzinski and Kernig signs. Infectious signs and symptoms include fever, tachycardia, chills, and malaise. A petechial or purpuric rash can occur in meningococcal meningitis. Projectile vomiting, nausea, decreased level of consciousness, seizures, and cranial nerve dysfunction are neurological signs of meningitis. Dementia is often the first sign of fungal meningitis. (McCance & Heuther, 2019).
Diagnosis
Diagnosis of meningitis is made with a physical exam, history, blood and CSF analysis and cultures, and imaging. Figure 4 details the initial management of a patient presenting with suspected meningitis. A definitive diagnosis of meningitis can be difficult to make as the clinical manifestations can vary in form and severity. Because of the variances in clinical presentation all patients that present with symptoms concerning for meningitis should undergo a lumbar puncture to obtain CSF for analysis and culture. However, due to the risk of increased intracranial pressure, The Infectious Disease Society of America recommends patients with signs of increased ICP undergo a CT Scan before lumbar puncture to help reduce the risk of herniation (Mount & Boyle, 2017). The results of the CSF analysis will vary depending on the microorganism that is causing the infection. Figure 5 details the typical CSF findings found in the different types of infectious meningitis.
Figure 4. Algorithm For Initial Management of Suspected Acute Meningitis (Am Fam Physician, 2017)

Figure 5. Typical CSF Parameters in Patients with Meningitis (Am Fam Physician, 2017)

Figure 4 and 5 retrieved from https://www.aafp.org/afp/2017/0901/p314.html