Normal Physiology
Normal physiology of patient’s mood, perception, emotion and behavior focuses majorly on neurotransmitters in the brain. There are over 46 neurotransmitters in the brain and many have more than one function. Neurotransmitters are chemical messengers that are released and received by synapses of neurons to mediate intracellular communication in the nervous system. They use electrical signals to stimulate messages along the neurons where it affects ion channels and eventually performs a specific mechanism at a site of action (McCance & Huether, 2014).
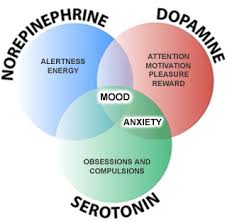
Serotonin is involved with mood, happiness, anxiety, and sleep induction. Raphe-Serotonin System normally modulates homeostasis, emotionality, and tolerance to aversive experiences. Norepinephrine in the brain helps regulate alertness, mood, functions in dream sleep, and maintains arousal. It also can help in the response to stressful situations. The locus ceruleus has a group of norepinephrine containing cells implicated in global psychologic processes including attention, vigilance and orientation to stimuli. Dopamine in the brain regulates reward and motivation which could explain the loss of interest in patients with depression. Dopamine motivates people to take action toward goals, desires, and needs, and issues a surge of reinforcing pleasure once they’ve been accomplished (Garcia-Arocena). Sufficient levels are needed for the brain to function properly and decreased levels have been found in patients with depression (McCance & Huether, 2014).
Major Depressive Disorder
Major depression is classified as a unipolar mood disorder. Further, major depression can be classified as when an emotional state, such as sadness, becomes chronic and uncontrollable. It is the most common mood disorder (McCance & Huether, 2014). Mood disorders are still being studied due to the unclear nature of how they occur due to the difficult availability of human brain tissue for neurochemical measurement until patients are post-mortem. Each of the dysfunctions below focuses on what are thought to be the causes of major depressive disorder.
Pathophysiology: Genetic Predisposition and Environmental Influences
There is a genetic predisposition in major depression that runs in families. However, due to the large variance in symptoms, developmental and environmental factors also must be evaluated in the contributing factors to major depression. One view of mood disorders includes the connection between susceptible genes and environmental influence. The combination of life stressors and a potentially dysfunctional serotonin (5-HT) system. The serotonin transporter serves in the reuptake of serotonin at the synapse and may moderate the serotonergic response to stress. Individuals with 2 copies of the s allele were more likely to develop major depression and have suicidal thoughts in response to stressors than individuals homozygous for the l allele. As well as, individuals with 2 s alleles increased their risk for major depression episodes by twofold after experiencing 4 or more stressful events (McCance & Huether, 2014).
Pathophysiology: Neurochemical dysregulation
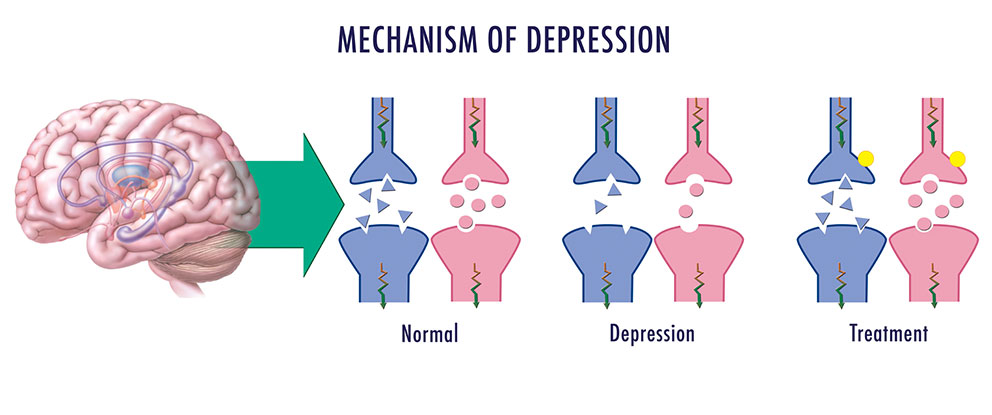
There are antidepressant drugs that can increase neurotransmitters in the body leading to another theory called the monoamine hypothesis of depression. In this hypothesis, there is a deficit in the concentration of the brain norepinephrine, dopamine, and/or serotonin resulting in depression. Antidepressant therapies focus on increasing the monoamine neurotransmitter levels within the synapses (McCance & Huether, 2014).
Pathophysiology: Neuroendocrine Dysregulation
There are 2 theories in the pathophysiology of depression that involve dysregulation of the neuroendocrine system. The first one focuses on stress and the hypothalamic-Pituitary-Adrenal system. The hypothalamic-pituitary-adrenal system (HPA) plays an essential role in an individual’s ability to cope with stress. Chronic activation of the HPA system and chronic glucocorticoid secretion are found in 30-70% of individuals with major depression suggesting the correlation between the dysfunctional system and depression. Chronic cortisol release in the body results in secretion of pro-inflammatory cytokines which causes immunosuppression and inflammation. Also, there is a Neurotrophic Hypothesis of depression. It is thought to focus on neuronal atrophy of the hippocampus resulting in no cell growth consequently causing in a reduction of the hippocampal brain derived neurotrophic factor (BDNF) and has been proposed as an extension of the monoamine hypothesis of depression.
The second neuroendocrine dysregulation is in the hypothalamic-pituitary-thyroid system. While this dysfunction is not completely understood, 20-30% cases of major depression have shown to have an altered hypothalamic-pituitary-thyroid (HPT) system. There is an increase in thyrotropin releasing hormone, blunted thyroid stimulating hormone in response to TRH challenge and decreased nocturnal rise in TSH level that normally occur. This all increases risk for relapse (McCance & Huether, 2014).
Pathophysiology: Neuroanatomic and Function Abnormalities
Depressed individuals post-mortem brains have shown widespread decrease in serotonin 5-HT1a receptor subtype binding in the frontal, temporal, and limbic cortex as well as serotonin transporter binding in the cerebral cortex and hippocampus, reflecting a dysfunction in the raphe-serotonin system. The activation of the locus ceruleus-norepinephrine system is capable of inhibiting the raphe-serotonin system. This suggests an indirect role in the modulation of serotonin function. Norepinephrine receptor alterations are found in the frontal cortex of some suicide victims with depression. Alterations in norepinephrine systems may be linked to attention or concentration difficulties as well as sleep and arousal disturbances in depression
Alterations in frontal and limbic regions (such as the amygdala) have shown a decreased number of glial cells in people with unipolar disorders. As well as, a decreased prefrontal cortex functioning and decreased frontal lobe volume.
Depressed individuals have also been found to have abnormalities in Cerebral blood flow and glucose metabolism. Dorsolateral prefrontal abnormalities in depression may be responsible for the retardation in cognitive processing and speech deficits similar to those found in schizophrenia. Dorsomedial frontal dysfunction may be associated with mnemonic and attentional impairments that accompany mood disorders. The frontal brain has increased blood flow and metabolism. It is positively related to negative affect in depressed individuals (McCance & Huether, 2014).
Clinical Manifestations/Diagnostic Criteria
To diagnosis depression, symptoms must be present for at least two weeks. There are unremitting feelings of sadness and despair. Depressive episodes may occur or recur suddenly, gradually or continue from a few weeks to months. Twenty percent of all people with depression exhibit chronic forms of depression. Symptoms vary widely depending on the individual. The timing and length of the depression also varies.
To be diagnosed with Major Depressive Disorder, patients have to have several, usually five or more, symptoms including low mood that is present for at least two weeks (Depression, 2018). Other symptoms of major depressive disorder include:
- Depressed or irritable mood
- Loss of interests and pleasures – this includes interpersonal relationships
- Significant weight gain or loss (5%) in a month
- Sleep Disturbances: Insomnia/Hypersomnia
- Psychomotor agitation or retardation: Restlessness or agitation can occur
- Fatigue or loss of energy
- Feelings of worthlessness or excessive guilt: Pessimistic/Negative outcomes are perceived
- Poor concentration or indecisiveness
- Recent thoughts of suicide/death: Suicidal risk increases with depression
Images:
Garcia-Arocena, D. (n.d.). Happy or SAD: The chemistry behind depression. Retrieved October 29, 2018, from https://www.jax.org/news-and-insights/jax-blog/2015/december/happy-or-sad-the-chemistry-behind-depression
LA NEUROSCIENZA DEL CERVELLO CON ADHD. (2018, September 17). Retrieved from https://mondoadhd.blog/2018/09/17/la-neuroscienza-del-cervello-adhd/
(n.d.). Retrieved October 29, 2018, from https://www.nature.com/articles/nrdp201665/figures/3
What are neurotransmitters? (2017, November 09). Retrieved from https://qbi.uq.edu.au/brain/brain-physiology/what-are-neurotransmitters