PM&R is not a field of medicine that I was familiar with coming in to medical school. The early favorite for me was orthopaedic surgery. I had shadowed surgeons in undergrad and had always wanted to work with athletes. I thought ortho would be the perfect fit. The Medical Specialty Preference Inventory (MSPI) is a tool designed to help medical students identify specialties that match their interests. The survey itself is about 40 items long and takes about 10-15 minutes to complete. It was no surprise that my MSPI results from my first semester of med school (pictured below) strongly indicated a preference towards ortho.
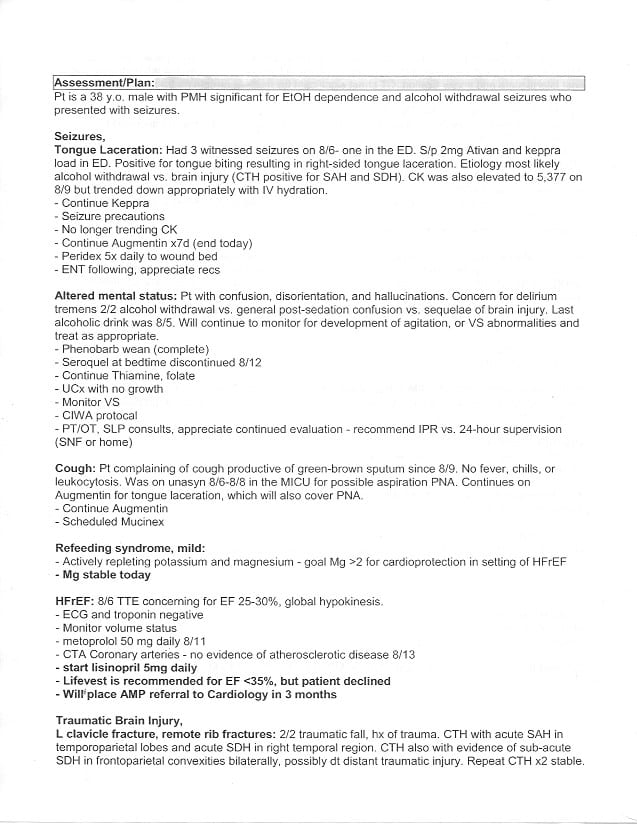
However, as time went on my preferences for what I want in a specialty evolved and new interests emerged. Although surgical procedures still interested me, I became more invested in the patient’s story and curious about how their life would change after surgery. On my neurology rotation I cared for patients who suffered from strokes, altered mental status, seizures, and weakness. The most we could do in the acute setting was make a diagnosis and stabilize them medically prior to discharge. I found myself wondering what was next for those patients and if they would ever be able to function at the level they had prior. When one of my patients required an EMG, I saw that there were two options for the consult: Neurology or PM&R. I had no idea that PM&R physicians performed EMGs and I became curious about what else fell into the scope of practice of a physiatrist. After doing more research about the field I was intrigued enough to schedule an elective rotation at my school’s inpatient rehabilitation hospital. I spent 2 weeks on the Stroke service working with a small team of just myself, the attending and a PGY2. After those two weeks, I was sold on PM&R! Shortly after completing the elective, I decided to repeat the MSPI. I think the results of that MSPI are very telling (see below).
With a firm dedication to a future career in physical medicine and rehab, I scheduled two, back-to-back rotations at Dodd Rehabilitation Hospital (OSU’s acute rehab hospital) at the outset of my fourth year. I spent one month each on the spinal cord injury (SCI) and traumatic brain injury (TBI) services. My month of SCI resulted in a Dean’s Letter of Commendation (below), and my elective in TBI resulted in a grade designation of Honors!
I’d like to highlight a quote from the evaluation above:
“Ms. Johnson has been an invaluable member of the SCI team at Dodd Hall. She numbers among the best medical students I’ve worked with, and she is going to make an excellent physician & physiatrist in the future”
In addition to my two rotations at Dodd, I wanted to see how other PM&R programs are run and how the culture of those programs may differ in other regions of the country. I was accepted to attend away rotations at the University of Pennsylvania and Thomas Jefferson University this fall, and I can’t wait to get back to seeing PM&R patients. As a further indication of my commitment, I joined the American Association of Physical Medicine and Rehabilitation as a student member, and began receiving the PM&R journal in order to stay up-to-date on current advances in the field.
I haven’t yet decided if I’ll pursue a fellowship after residency. As of now, I have interests in sports medicine, TBI, spine, and peds. Although I’m not set on any one specialty, I like the idea of performing in-office procedures. I imagine practicing at either an academic institution or a multidisciplinary practice along with professionals in other, related fields of medicine. I hope to attend a well-rounded residency program that treats a wide spectrum of conditions and will provide ample opportunity for me to explore my many interests. I’m also looking for a program with residents who are active in the community. Most importantly, I want to be a part of a program with a “tight-knit” group of residents and program leadership that is supportive and invested in the success of the residents.