Image Reference: https://blog.ekincare.com/2018/06/29/diagnosis-of-hypertension/
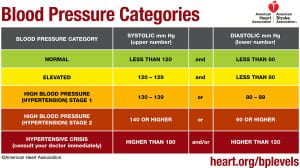
Hypertension or high blood pressure, is when an individual has consistently high arterial blood pressure, also known as the force with which blood flows through a person’s blood vessels (McCance & Huether, 2019). A normal blood pressure reading is a systolic (upper) number lower than 120 mmHg and a diastolic (lower) number that is lower than 80 mmHg (American Heart Association, 2017). Elevated blood pressure is when the systolic (upper) number is 120-129 mmHg with a normal diastolic (lower) number (American Heart Association, 2017). Stage one high blood pressure or hypertension is when the systolic (upper) number is between 130 mmHg and 139 mmHg and the diastolic (lower) number is between 80 and 89 mmHg (American Heart Association, 2017). The second stage of hypertension or high blood pressure is when the systolic (upper) number is 140 mmHg or higher and the diastolic (lower) number is 90 mmHg or higher (American Heart Association, 2017).
For someone to be diagnosed with hypertension their blood pressure measurements have to be taken two separate times that are at least two minutes apart, with the person seated, arm supported at heart level, with the person having rested for at least five minutes, and they should not have been smoking or drank any caffeine in the last 30 minutes (McCance & Huether, 2019). For hypertension to be diagnosed the diastolic and systolic numbers of the two readings are averaged and that measurement are found to be high according to the numbers above (McCance & Huether, 2019). Hypertension is often called a silent disease because in its early stages, there are commonly no other clinical manifestations besides high blood pressure measurements (McCance & Huether, 2019).
Hypertension is thought to be caused by both genetic and environmental factors (McCance & Huether, 2019). Genetic variations that cause the sympathetic nervous system (SNS) or the renin-angiotensin-aldosterone system (RAAS) to be overactive predispose a person to hypertension (McCance & Huether, 2019). Additionally, genetic modifications in the function of renal sodium excretion, sensitivity to insulin, and sodium and/or calcium transport can also contribute to an increased risk for hypertension (McCance & Huether, 2019). Some environmental factors that increase the risk for hypertension include diet, exercise, and smoking (McCance & Huether, 2019).
There are two mechanisms by which blood pressure can be increased: an increase in vascular resistance, an increase in cardiac output, or both (McCance & Huether, 2019). Cardiac output increases when stroke volume or heart rate increases and vascular resistance is increased by vasoconstriction or when the blood becomes thicker (McCance & Huether, 2019). Many pathophysiologic processes are involved in facilitating the maintenance of these mechanisms.
The renal excretion of sodium is one of these processes. Blood volume increases when the renal system excretes less salt due to water retention, thus increasing stroke volume and consequently blood pressure (McCance & Huether, 2019). When this system functions normally, the kidneys excrete the appropriate amount of salt to maintain, but not increase blood pressure. Those with hypertension are more likely to secrete less sodium in their urine at any given blood pressure (McCance & Huether, 2019).
The sympathetic nervous system (SNS) also helps modulate blood pressure by stimulating cardiac contractility and prompting vasoconstriction (McCance & Huether, 2019). It does so by controlling the release of epinephrine and norepinephrine which can bind to either alpha 1 receptors that reside on peripheral blood vessels or beta 1 receptors that reside on cardiac tissue (McCance & Huether, 2019). When this system functions normally, these catecholamines are released in the appropriate amount and interact with their receptors properly. In those with hypertension, there may be an increase in production of these catecholamines or their receptors may be especially reactive (McCance & Huether, 2019). This increased SNS activity triggers the heart rate to increase when affecting the beta 1 receptors and peripheral vasoconstriction when affecting the alpha 1 receptors (McCance & Huether, 2019). Both of these functions raise blood pressure (McCance & Huether, 2019).
There is also a connection between the sympathetic nervous system and kidney function. SNS activity triggers the release of renin, increases the amount of sodium that is reabsorbed, and lowers blood flow to the kidneys (McCance & Huether, 2019).
Another system that affects blood pressure and can contribute to hypertension is the renin-angiotensin-aldosterone system (RAAS). When this system functions normally, renin is released by juxtaglomerular cells in the kidney in response to increased SNS activity as well as in response to low blood pressure or low sodium as detected by macula densa cells (McCance & Huether, 2019). Renin goes on to convert angiotensinogen into angiotensin I (McCance & Huether, 2019). Subsequently, angiotensin-converting enzyme (ACE) is secreted by the lungs and converts angiotensin I to angiotensin II, which has vast effects on blood pressure modifying processes (McCance & Huether, 2019). Angiotensin II increases SNS activity; triggers the adrenal gland to secrete aldosterone, which causes water retention; prompts arterial vasoconstriction; activates anti-diuretic hormone (ADH); and causes the myocytes of the heart to hypertrophy (McCance & Huether, 2019). In those with hypertension, the whole RAAS system is overactive which increases angiotensin II and exacerbates its effects resulting in increased blood pressure.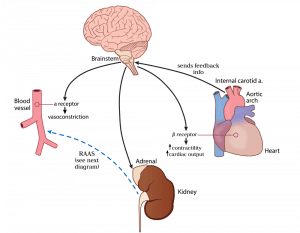
Image Reference: https://hasshe.com/vasodilation-nicotine-5c148fe58719620724c2bbfa/
Hypertension can be affected by inflammation (McCance & Huether, 2019). Injury to endothelial cells, or the cells that line the inside of blood vessels, along with lack of good blood supply to tissues in the body can trigger the immune system to release substances which directly impact the actions of the blood vessels (McCance & Huether, 2019). In a normal short-term injury, the appropriate substances (vasoactive cytokines) are released and help to heal the injured cite without causing overall harm to the body (McCance & Huether, 2019). When an injury to endothelial cells lasts a long time or becomes chronic, the cytokines can cause permanent damage resulting in a change in structure that prevents cells from functioning normally (McCance & Huether, 2019). This permanent change often leads to decreased production of vasodilators, or substances that the body produces to relax the blood vessels (nitric oxide) and an increased production of vasoconstrictors, or substances that the body produces to tighten blood vessels and increase blood pressure (McCance & Huether, 2019). This combination of events leads to an overall increase in blood pressure (McCance & Huether, 2019).
Insulin resistance is commonly associated with hypertension (McCance & Huether, 2019). Insulin resistance occurs when the body has a decreased response to insulin (McCance & Huether, 2019). Insulin is a hormone which normally acts in the body to stabilize blood sugar levels, and in doing so, interacts appropriately with other substances in the body to maintain a normal balance of vasodilators, salt and water (McCance & Huether, 2019). When someone is insulin resistant, there is an associated decrease in release of vasodilators (substances that decrease blood pressure) by endothelial cells (McCance & Huether, 2019). Insulin resistance impacts kidney function which leads to salt and water retention (McCance & Huether, 2019). Overactivity of the SNS and RAAS is also common in patients with insulin resistance (McCance & Huether, 2019). In some patients with diabetes, effective management of blood sugar levels can decrease blood pressure (McCance & Huether, 2019).
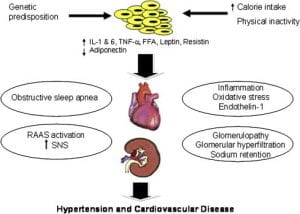
Obesity can have a major impact on hypertension (McCance & Huether, 2019). Obesity is associated with increased inflammation, activation of the RAAS and SNS, insulin resistance, as well as kidney and endothelial cell dysfunction (McCance & Huether, 2019). All these phenomena, as discussed above on this page, cause blood pressure levels to rise (McCance & Huether, 2019). Obesity causes changes in the fat tissue’s secretion of adipokines (McCance & Huether, 2019). Normally, adipokines are substances released by fat cells that act to regulate the actions of the fat cells and the tissues which the cells make up (McCance & Huether, 2019). When an individual is obese, there is an associated resistance to the action of an adipokine called leptin (McCance & Huether, 2019). In most individuals without obesity, leptin acts in the fat tissue to reduce the overall weight and fat content in a person (McCance & Huether, 2019). Under normal circumstances, the use of leptin by fat cells leads to its uptake from the blood into cells. In obese individuals, the decreased use of leptin by fat cells leads to an increase in the amount of leptin left circulating in the blood (McCance & Huether, 2019). This increase in leptin levels in the blood cause an increase in SNS activity and affect the kidneys in such a way that leads to less filtering of sodium out of the body (McCance & Huether, 2019).
Image Reference:
Kurukulasuriya, LR., MD, Stas, S., MD, Lastra, G., MD, Manrique, C., MD and Sowers, J.R., MD. (1 September 2011). Hypertension in Obesity [diagram]. Retrieved from: https://www-clinicalkey-com.proxy.lib.ohio-state.edu/#!/content/playContent/1-s2.0-S0025712511000629?returnurl=https:%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS0025712511000629%3Fshowall%3Dtrue&referrer=
Levels of adiponectin, a protein made by fat tissues, are reduced in obese individuals (McCance & Huether, 2019). This lack of a normal adiponectin level is associated with insulin resistance, decreased nitric oxide (a vasodilator that decreases blood pressure), and an increased activation of the SNS and RAAS (McCance & Huether, 2019). These factors lead to overall constriction of the blood vessels, retention of excess water and salt in the body, and kidney dysfunction (McCance & Huether, 2019). All of these lead to a rise in blood pressure (McCance & Huether, 2019).
Secondary hypertension is when high blood pressure is caused by another disease or medication (McCance & Huether, 2019). Primary hypertension is caused by a combination of one or more factors explained above. Some things that can cause secondary hypertension include kidney disease, tumors associated with the adrenal gland, and medications such as oral contraceptives, antihistamines and corticosteroids (McCance & Huether, 2019). The cause can be identified and treated or removed to lower blood pressure (McCance & Huether, 2019).