Criteria for Diagnosis
HbA1c ≥ 6.5%
Fasting plasma glucose (FPG) ≥ 126 mg/dL
2 hour plasma glucose ≥ 200 mg/dL during an oral glucose tolerance test (OGTT)
In a patient with classic symptoms of hyperglycemia, a random plasma glucose ≥ 200 mg/dL
Treatment
Treatment of type 2 diabetes mellitus (T2DM) focuses on decreasing blood glucose, increasing insulin secretion, or countering insulin resistance. Treatment of symptoms, such as diabetic retinopathy, nephropathy, or neuropathy requires additional and involved patient education, medications, and therapies.
Lifestyle Modifications
Treatment of obesity and other symptoms of metabolic syndrome is essential. Exercise is an effective intervention because it reduces postprandial blood glucose levels, diminishes insulin requirements, lowers triglyceride and cholesterol levels, and increases the level of HDL cholesterol. Physical activity also aids in weight reduction. Diet modifications include restricted yet consistent caloric intake appropriate for ideal weight and activity level. Dietary counselling is through medical nutrition therapy (MNT) should focus on achieving biometric goals (McCance & Huether, 2014).
Getty Images; Shutterstock; Michael Phillips/Getty Images
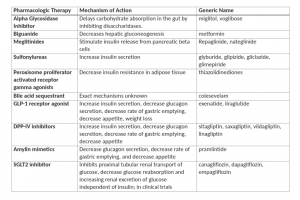
Pharmacological Interventions
Oral hypoglycemic medications are usually needed for optimal management of T2DM.
Insulin may be need in later stages due to functional loss of beta cells of the pancreas (McCance & Huether, 2014).
Surgery
Bariatric surgery may be indicated for patients who are morbidly obese and unresponsive to diet and exercise interventions. Currently, powerful evidence exists that shows bariatric surgery improves glycemic control in up to 80% of individuals with T2DM even before there is any significant weight loss (McCance & Huether, 2014).