The lungs are the main organ of the respiratory system. Their main function is to assist in the exchange of oxygen and carbon dioxide using the air that we inhale (McCance & Huether, 2019). The right lung has three lobes and the left lung has two lobes. The pulmonary artery brings deoxygenated blood to the capillaries that form respiratory membranes with the alveoli (McCance & Huether, 2019). The alveoli will perform gas exchange, and then the pulmonary veins will return the now oxygenated blood back to the heart so that it can be sent throughout the body (McCance & Huether, 2019). Around the lungs is the pleura which is made up of two layers, the visceral and parietal pleural layers. Between these two layers there is a small amount of pleural fluid that works as a lubricant to prevent any friction, as well as an adhesive to bring the lungs to the thoracic wall so that it can assist in the movement of lungs with every breath (McCance & Huether, 2019). With normal lung function, the alveoli in the lungs have strong elastic walls that allow air to expand and contract the little sacs. The bronchioles are nice and clear and allow air to flow in and out of them smoothly (McCance & Huether, 2019). This is normal lung function.
COPD is Chronic Obstructive Pulmonary Disease. This is a lung disease that is obstructive in nature, irreversible, and can get worse over time (McCance & Huether, 2019). COPD is a common disease that is preventable. There are two main conditions that cause COPD. One is emphysema, and the other is chronic bronchitis. In some situations, you may find a genetic susceptibility such as in the case of alpha-1 antitrypsin deficiency (McCance & Huether, 2019). COPD is the third leading cause of death in the United States and the sixth leading cause of death worldwide (McCance & Huether, 2019).
COPD happens when the lungs are exposed to harmful particles and gases which cause the lungs to have an abnormal inflammatory response (McCance & Huether, 2019). The most common harmful cause is cigarette smoking. COPD can also occur from exposure to occupational dusts and chemicals, indoor air pollution (such as fuels used for cooking and heating), outdoor air pollution, any factor involved in lung growth during gestation and childhood, and genetic susceptibilities such as a mutation in the alpha-1 antitrypsin gene (McCance & Huether, 2019). In both chronic bronchitis and emphysema you will see involvement of neutrophils, macrophages, and lymphocytes to the lungs, which will lead to inflammation, oxidative stress, extracellular matrix proteolysis, and apoptotic and autophagic cell death, all of which cause progressive damage (McCance & Huether, 2019).
Chronic bronchitis is one type of COPD. In chronic bronchitis, patients exhibit a chronic productive cough and experience excess mucus build up that leads to irritation and mucus throughout the large and small airways of the lungs (McCance & Huether, 2019). The lining within the airways becomes swollen and irritated and the cilia function becomes impaired, making it harder to breathe. This happens for at least three months of the year and for at least two years in a row. These patients will end up with a ventilation-perfusion mismatch with hypoxemia (Department of Pulmonary Rehab, 2009).
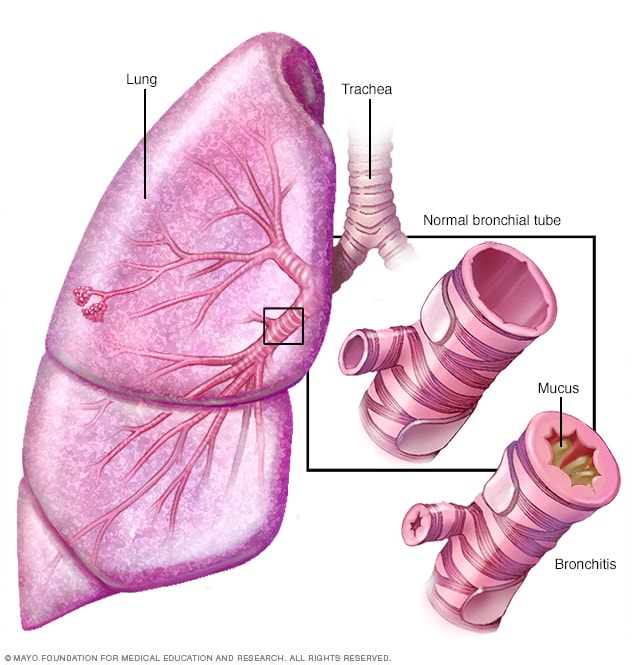
Imagine retrieved from mayoclinic.org
Emphysema is a second type of COPD. It is a disease of the alveoli. In emphysema, there is irritation to the alveoli in the lungs which eventually leads to damage and a reduction of air exchange in the lungs (McCance & Huether, 2019). This makes it hard for the patient to be able to move oxygen into the blood or take carbon dioxide out of the blood. Patients with emphysema will have permanent enlargement of the gas-exchange airways as well as damage to the walls of the alveoli (McCance & Huether, 2019). They lose their normal elasticity that allowed them to expand and contract, letting air in and out as with normal, healthy alveoli (Department of Pulmonary Rehab, 2009).
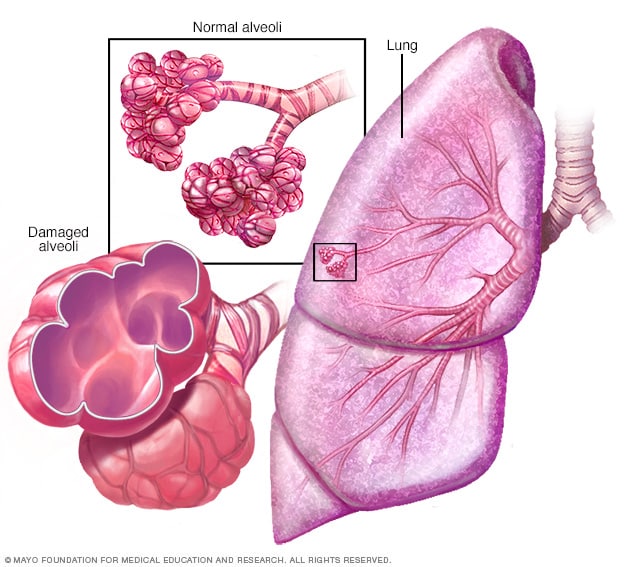
Imagine retrieved from mayoclinic.org
Clinical Presentation:
Often with COPD, patients you will see some combination of both presentations seen in chronic bronchitis and emphysema.
In review, COPD causes the flow of air out of the lungs to be blocked. The air is therefore trapped in the lungs, making it hard for the lungs to send the right amount of oxygen to the rest of the body (McCance & Huether, 2019). Patients can breathe air in, but getting air out is a challenge. Often, these patients will present with coughing (which can be productive or nonproductive), wheezing, shortness of breath that gets worse with exertion, and feelings of tightness in the chest (Department of Pulmonary Rehab, 2009).
The main causes of COPD are smoking, exposure to secondhand smoke, and working in environments where you are breathing in toxic dusts, fumes or gases (McCance & Huether, 2019).
Patients with COPD need to understand that this disease is chronic, obstructive in nature, and progressive over time. This means that they cannot reverse the disease, but they can stop it in its tracks and keep it from getting worse. One of the best ways to do this is to stop smoking if the patient is a smoker (Department of Pulmonary Rehab, 2009).