Differential Diagnosis I
Allergic Alveolitis (Hypersensitivity Pneumonitis)
Rationale
Acute allergic alveolitis, also known as hypersensitivity pneumonitis, is a diagnosis to be considered in this patient. The patient presents with dyspnea, elevated temperature and cough, all symptoms that are present when evaluating for allergic alveolitis. In order to have onset of allergic alveolitis, there needs to be a repeated inhalation of organic particles or fumes, causing an allergic or inflammatory process within the lungs (McCance & Huether, 2019). The hypersensitivity type III response is then activated as part of the pathological process involved in allergic alveolitis. Given the history of recent home renovation, there could be an inflammatory process associated with the exposure to the chemical or fumes in the paint or from the dust.
Although allergic alveolitis could be a potential diagnosis for this patient, there are some other parts of her history and assessment to consider. On her lung exam, the nurse practitioner notes expiratory wheezing, a symptom not associated with allergic alveolitis. Typically with allergic alveolitis, you will hear bibasilar crackles on the lung exam (Wuyts, Sterclova, & Vasakova, September 2015). Additionally, although the patient was exposed to fumes related to home renovation, her family history of asthma, a current respiratory tract infection, and wheezing episodes in the past that were responsive to a bronchodilator (albuterol), would align more with the diagnosis of asthma.
Figure 1 Hypersensitivity Pneumonitis (Pain Assist, 2019)

Differential Diagnosis II
Acute Bronchitis
Rationale
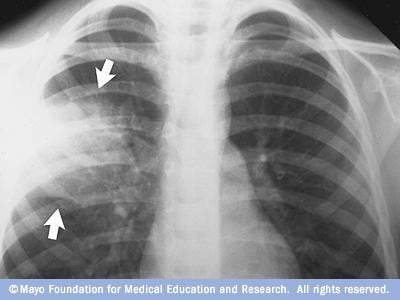
Due to our patient presenting with an intermittent productive cough, low grade fever, chest tightness and dyspnea, acute bronchitis should be considered as a differential diagnosis. Acute bronchitis is defined as active inflammation or an infection occurring in the lower airways (as seen in Figure 1) causing a low-grade fever in most patients (McCance & Huether, 2019). Depending on whether the bronchitis is caused by a virus or bacteria, a productive or non-productive cough can be seen. Paroxysmal coughing, or constant, forceful coughing can be seen with acute bronchitis leading to chest pain or tightness and dyspnea following the coughing spells (McCance & Huether, 2019). In our patient, paroxysmal coughing could be brought on from the remaining dusty air after their recent home renovation.
Although some aspects of our patient’s history is consistent with acute bronchitis, some aspects cannot be related to this diagnosis. Wheezing is not often seen with acute bronchitis except in patients with an already known history of asthma or COPD. Our patient also presents in acute respiratory distress as she is showing shortness of breath with speaking. Typically, acute bronchitis will not lead to respiratory distress except the dyspnea that is seen after paroxysmal coughing occurs (McCance & Huether, 2019).
Figure 2 Acute Bronchitis (MedlinePlus, 2019)
Differential Diagnosis III
Pneumonia
Rationale
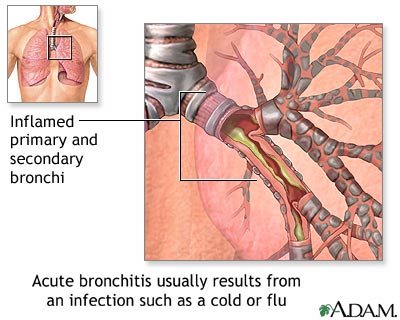
Pneumonia is another infectious process of the lower airways of the lungs that should be considered as a potential diagnosis for this patient. Our patient’s history includes a recent upper respiratory infection which commonly occurs before an individual develops pneumonia (McCance & Huether, 2019). Our patient’s elevated temperature, intermittent productive cough and dyspnea as evidenced by her respiratory rate of 40, and shortness of breath while speaking is also consistent with a diagnosis of pneumonia (McCance & Huether, 2019). A chest x-ray would need to be performed to confirm a diagnosis of pneumonia that shows evidence of consolidation in the lungs, as seen in Figure 2.
Although pneumonia could be considered as a potential diagnosis for this patient, there are some findings on the patient’s exam and clinical history to consider. As previously mentioned, the nurse practitioner noted that the patient has expiratory wheezing, a symptom not found in pneumonia. Typically on auscultation in a patient who has pneumonia, you will hear inspiratory crackles and decreased breath sounds (McCance & Huether, 2019). Additionally, a low-grade fever is often seen in patients with asthma, as evidenced by the patient’s temperature of 100.8ºF. However, in pneumonia, especially bacterial pneumonia in children, you will see much more elevated temperature indicting there is an infectious process (McCance & Huether, 2019).
Figure 3 Chest X-ray of Pneumonia (Mayo Clinic)