Differential Diagnosis I: Pneumonia
Pathophysiology
- Aspiration of secretions is the most common route;
- Can cause of a lower respiratory infection.
- Additional route of contamination: inhalation of a microorganism released by another person through coughing or sneezing.
- Endotracheal tubes can have a biofilm of bacteria acquired through suctioning.
- It is the 8th leading cause of death in the United States (McCance & Huether, 2019).
Clinical manifestations (resembling asthma)
- Dyspnea
- Coughing
- Chest pain
- Fever
- Productive or nonproductive cough
- Treatment: correcting ventilation and oxygenation first (McCance & Huether, 2019).
Rationale
- Pneumonia is caused by a bacteria or aspiration, but asthma is not caused by either.
- It is treated through antibiotics, versus corticosteroids and bronchodilators.
- Pneumonia can lead to septic shock.
- Sputum culture tested negative for this patient case.
- Chest x-ray would show consolidation or infiltrates if the diagnosis was pneumonia.
- In this case the results showed bronchial thickening, hyperinflation, and focal atelectasis.
- Pulmonary function tests (PFT) are used to diagnose asthma when patient is not in severe distress.
- Pneumonia is an infection of the lower respiratory tract due to bacteria, viruses, protozoa, fungi, or parasites.
- Risk Factors
- Weak or compromised immune system.
- Already diagnosed underlying lung disease such as COPD, difficulty swallowing, immobilized, or being intubated.
- Most cases are followed by a severe viral respiratory tract infection.
- Can be acquired in many ways; community, hospital, ventilator associated, and healthcare associated (McCance & Huether, 2019).
Diagnosis II: Croup (Acute Laryngotracheobronchitis)

Pathophysiology
- Inflammation from vocal cords to the bronchioles from Influenza A or a respiratory syncytial virus
- Westley Score= tool most often used to estimate the severity of croup which assesses:
- Stridor
- Retractions
- Air entry
- Cyanosis
- Dyspnea
- Level of consciousness (LOC) (McCance & Huether, 2019).
Clinical Manifestations (resembling asthma)
- Dyspnea
- Retractions
- Low grade fever
- This can occur with asthma when asthma is triggered from a virus
- Coughing
- No treatment for mild symptoms
- Treatments for moderate-severe include injected steroids and inhaled glucocorticoids (McCance & Huether, 2019).
Rationale
- Conjunctivitis and nasal discharge from a respiratory virus.
- If patient was diagnosed with croup their neck x-ray would show a steeple sign for patients with moderate-severe symptoms.
- In asthma, typically no neck x-ray is ordered.
- Treatments for moderate-severe croup that are not used in asthma:
- Nebulizer racemic epinephrine stimulates alpha and beta adrenergic receptors
- To alleviate edema in mucosa
- Oxygen administration
- Not generally administered in asthma except in severe asthma exacerbation.
- Nebulizer racemic epinephrine stimulates alpha and beta adrenergic receptors
- Onset is usually caused by a virus or result of foreign body obstruction in the upper airway.
- Stridor = a harsh, barky cough heard when there is a tracheal foreign body obstruction.
- This is a classic symptom of an irritation in the upper airway
- In asthma, stridor is not heard.
- Generally, wheezing in the lower airways is present.
- Risk of croup:
- More frequently seen in younger children (6 months – 3 years old);
- Asthma cannot typically be diagnosed until 2 years old.
- Due to the smaller luminar openings and easily collapsible diameter;
- Decreased airway opening makes you prone to frequent upper airway obstructions (McCance & Huether, 2019).
- More frequently seen in younger children (6 months – 3 years old);
Differential Diagnosis III: Bronchiolitis
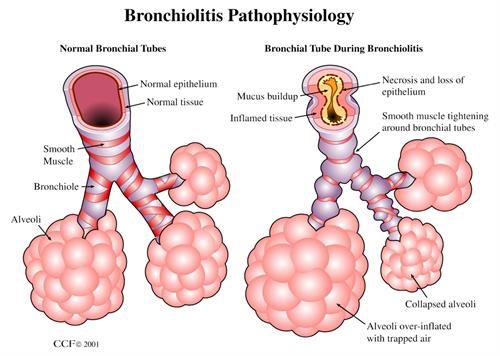
Pathophysiology
- V/Q Mismatch
- Bronchospasm
- Hypoxemia
- Air Trapping
- Increased functional residual capacity
- Decreased Lung Compliance (Cordell, 2019).
Clinical Manifestations (resembling asthma)
- Rapid respiratory rate
- Significant use of accessory muscles
- Dry, nonproductive cough
- Hyperinflated chest
- Wheezing upon auscultation of the chest (Cordell, 2019)
Rationale
- Low grade fever
- This can occur with asthma when asthma is triggered from a virus
- Rhinorrhea
- This can occur with asthma when asthma is triggered from a virus
- Decreased appetite
- Pulsus Paradoxus (Cordell, 2019).
- A respiratory tract infection of the small airways and bronchioles
- Developed by a virus, which causes diffuse inflammation
- Occurs mainly in infants and young toddlers.
- Can lead to an increased risk for asthma later in childhood
- Particularly affects those with a family history of asthma (McCance & Huether, 2019).