Alzheimer’s disease (AD) is characterized by two pathological lesions, beta-amyloid (Aβ) plaques and neurofibrillary tangles, that are progressively distributed throughout the brain. These lesions are associated with disruption of the communication pathways between neurons, neuron degeneration, brain atrophy, and functional loss. However, the specific etiology of AD remains uncertain (Sperling et al, 2011).

Photomicrograph of human brain with Alzheimer disease following Beilchowsky stain. The stain highlights an extracellular neuritic plaque (upper right) and an intraneuronal neurofibrillary tangle (lower left) (Up to Date).
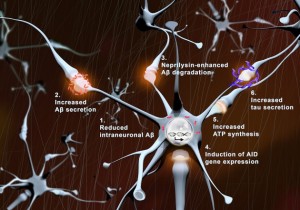
With synaptic activation: (1) intraneuronal levels of Aβ (red) are reduced, (2) Aβ secretion is augmented, (3) neprilysin-induced Aβ degradation is enhanced, (4) transcription of pro-survival genes (AID) increases, (5) local ATP synthesis rises at synapses, and (6) tau secretion is augmented (Tampellini, 2015).
Beta-amyloid plaques
The outer cell membrane of neurons contains an amyloid precursor protein (APP). In the normal brain, alpha-secretase and gamma-secretase cut APP into smaller protein fragments that are thought to be helpful to neurons and then later cleared from the brain. In AD, beta-secretase and gamma-secretase cut APP into small Aβ fragments. Researchers hypothesize that the Aβ oligomers disrupt neuronal cell signaling and communication at the synapses and later stick together to form beta-amyloid plaques (NIA, 2015). Researchers believe the beta-amyloid plaques may also trigger an inflammatory immune reaction that results in neuronal death. In early onset familiar AD, the formation of Aβ plaques is related to autosomal dominant mutations of the APP gene, presenilin 1, and presenilin 2 genes. Apolipoprotein E gene-allel4 may play a role in Aβ plaque formation in late onset AD (McCance & Huether, 2014).
Neurofibrilary tangles
Neurons have microtubules that transport nutrients and other substances. In the normal brain, tau proteins provide stability and keep the microtubules straight. In AD, tau proteins are hyperphosphorylated and disassociate from the microtubules. The tau proteins accumulate inside the neuron, forming neurofibrillary tangles that impede nutrient transport and disrupt communication (NIA, 2015). These tangles are toxic to the neuron and eventually contribute to neuronal death.
Video from http://ed.ted.com/lessons/what-is-alzheimer-s-disease-ivan-seah-yu-jun
Progressive Spread of Lesions and Stages of Disease
While both types of lesions result in cell death and brain atrophy, neurofibrillary tangles appear to spread throughout the brain in an orderly procession that corresponds to the stages of Alzheimers disease progression (Keene, et al, 2015). Neurofibrilary tangles begin in the hippocampus and then spread throughout the brain before finally developing in the medullary centers leading to death. (Granic, et. Al, 2010). Lesions can develop in the brain 10-20 years before symptoms appear and progression of the lesions throughout the brain can occur for as long as 10 years (NIA, 2015).
http://www.youtube.com/watch?v=9Wv9jrk-gXc