“Lo siento, no hablo español” (I’m sorry, I don’t speak Spanish)
“I wish I spoke Spanish,” I said to myself. “I seriously wish I did.”
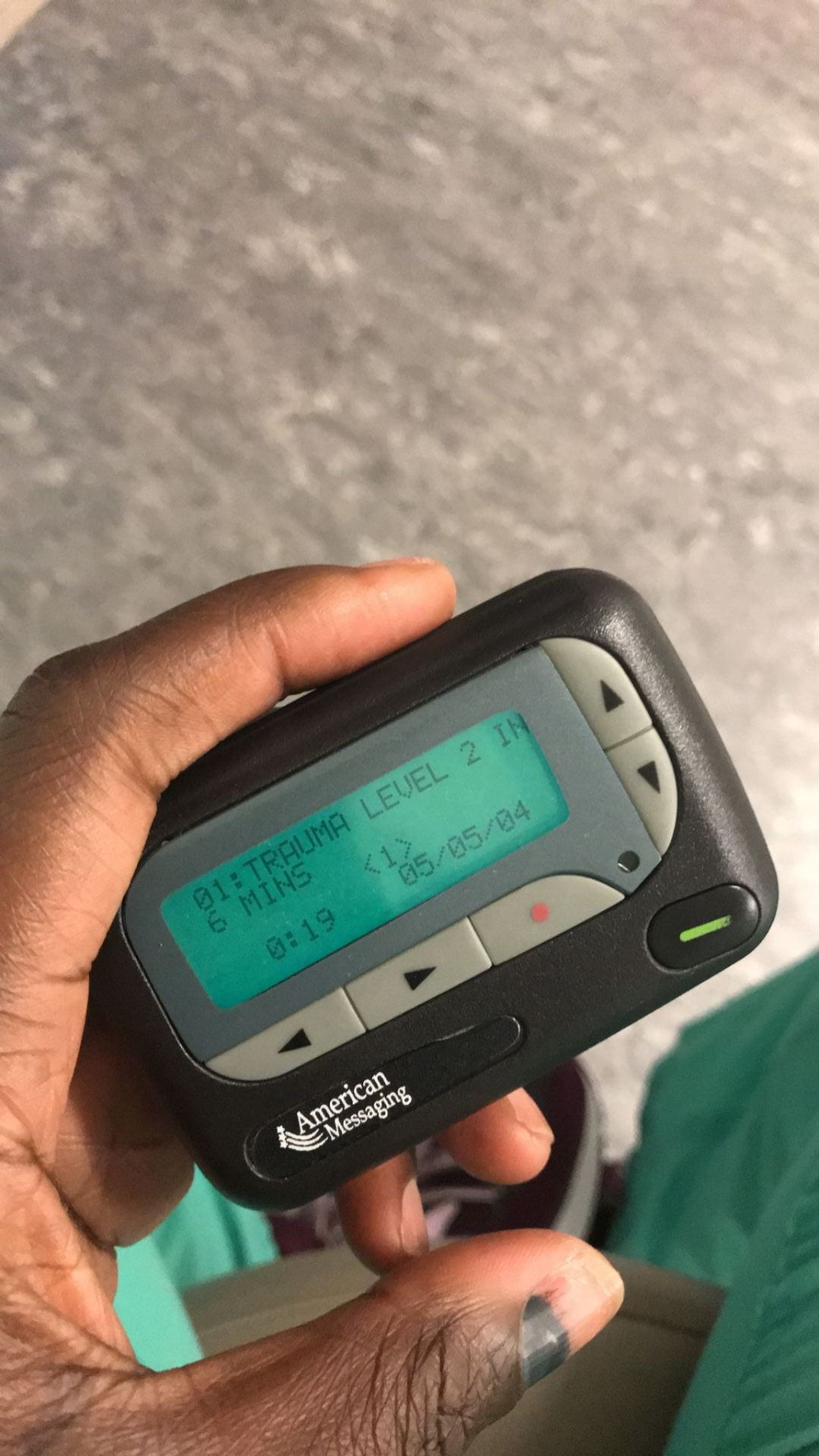
I was in the trauma bay, on my surgery rotation as a 3rd year, gowned up and ready with my trauma shears. A patient was being brought in by EMS team in 10 minutes. On the whiteboard was a description of the trauma incident, patient characteristics, possible injuries, and important vitals/ hemodynamic status – it was a motor vehicle accident, young female, no seat belt. In the midst of those words, something stood out to me – “Spanish speaking. Does not speak English.” For what was possibly the hundredth time in my life, I thought to myself, “Man, I wish I spoke Spanish.” I could hear my husband teasing me as he often those when we talk about Spanish, “Derin, how is it that you’ve been to Peru, El Salvador, Puerto Rico, and still don’t speak or understand Spanish? Are you even making an effort to learn?” He was fluent in Spanish and rightly could tease me about it. My excuse was always the same – I didn’t take Spanish in high school, and the little Spanish I pick up on my travels, I often forget once I’m no longer immersed in the country. Still, in this particular moment, here in the trauma bay, with a language barrier ever so imminent in such a critical situation, I couldn’t help but think, “Derin, you’ve seriously gotta learn Spanish.”
My senior resident saw the words on the board as well, looked around the room and said loudly, “Anyone speak Spanish in here? Anyone?” Thankfully, a 4th year medical student stepped forward, “I do!”
“Are you sure? Fluently?” My resident asked
“Yes, I’m fluent, “ the medical student responded
“Ok, perfect.”
I was relieved, as I imagined others in the room were. In the trauma bay, you need to act quickly, you need to be efficient. A language barrier can be detrimental in ensuring optimum ambulatory care. Asking if the patient is hurting anywhere, confirming allergies, and past medical conditions before obtaining CT images were critical. Unfortunately, waiting for MARTY machine (for language translation) is not ideal in an emergent situation like this.
Our patient arrived in a stretcher with a neck brace on due to possible C-spine injury. She had multiple abrasions, with some dried blood on her extremities, she looked visibly scared. As my resident began to run the trauma, and others in the room began checking the patient’s airway, breathing, and circulation, the 4th year medical student was also talking to patient in Spanish, explaining what was going on and asking pertinent questions.
It’s been a year since that incident and it’s stuck with me. No, I’m still not fluent in Spanish, but I’m fully aware that knowing even a little bit can be the difference between life and death in a critical situation. Therefore, my goal is still to learn basic medical Spanish. A significant population of the U.S. is Spanish speaking and being able to communicate effectively is part of providing excellent care. Though, I may never be fluent, I do believe in critical situation like above, been able to communicate even just the basic words are important.
As a fourth year and future resident, I anticipate that a similar situation like this will happen in the near future, likely multiple times over. I also recognize that communication is more than just language, even as a soon to be physician, its more than just communicating with patients. It also involves collaborating effectively with other healthcare team members, listening, observing, conducting timely documentation and even preparing and distributing educational materials to individuals and groups. I have had the privilege of doing all of this in the past 4 years. On my Ross ICU, I learned to communicate effectively on the critical status of my patients. In presenting my research at a national conference, I learned to communicate to members of the medical profession on my findings and the significance of it, and even on my trauma surgery rotation, when doing a secondary survey of a trauma patient, I learned to communicate clearly and effectively as well. As an incoming intern, I am confident in this competency, being also aware that there is room to improve. My goal, specifically, is to improve on my written documentation and verbal communication with Attendings.