Improving the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores has always been a challenge for US hospitals. Hospitals with poor HCAHPS scores can lose up to 2% of their Medicare reimbursements, which equates to a several million dollars for an average sized hospital. Using data from over 3615 hospitals between the years 2007-2014, we studied how hospitals improve their HCAHPS scores. We found that it is common from hospitals to use resources from their existing administrative offices such as office of quality and patient safety to improve HCAHPS but are less successful. This is because, elements of HCAHPS such as communication with the nurses and physicians are often considered less tangible and hence difficult to improve when compared to evidenced-based measures such as length of stay reduction. Performing well on HCAHPS therefore requires hospitals to change their operating routines and organizational culture. To accomplish these tasks, we found that a certain proportion of hospitals are undertaking a number of initiatives that are unique to this industry. One such initiative includes setting up the Office of Patient Experience (OPX). An OPX is generally tasked with developing and implementing best patient experience practices to ensure that the hospital delivers consistent patient-centered care. It is different from other entities such as “Patient Council” and “Patient Relations Office,” which historically have been responsible for interfacing with the patients, surveying patients and resolving patient issues. One example of this office and how it operates can be found at the Cleveland Clinic
Our Findings
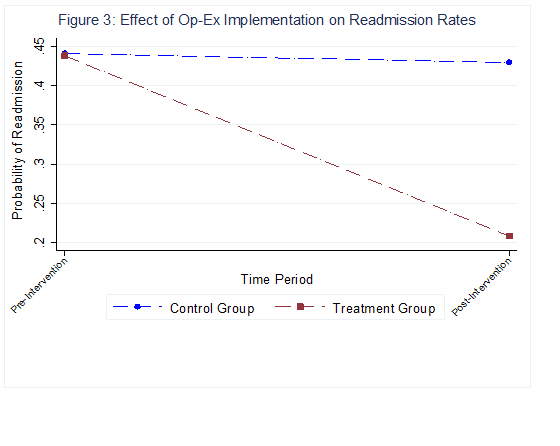
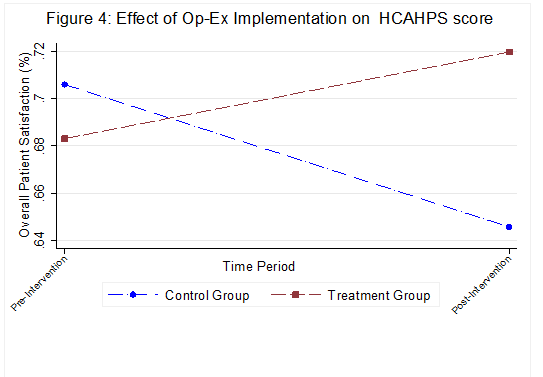
We collected extensive data on the setting up and operations of these offices in the US. Between 2007 and 2014, we found that there were 132 hospitals that had an OPX within their organizational structure. We also find that this number continues to grow in recent years. Our results suggest that hospitals with an OPX are associated with 1.95% higher HCAHPS for each year of operation. We also found that hospitals that have higher residents and treating high acute patients (measured using case mix index) benefit from these offices to manage patient and provider variations. Specifically, for hospitals with high CMI, we observe a 6.5% improvement in HCAHPS for each year increase in operation of the OPX, with no significant impact observed for hospitals with low CMI. Similarly, for hospitals with high resident intensity, we observe a 1.8% improvement in HCAHPS for each year increase in operation of the OPX, and only 0.9% improvement observed for hospitals with low resident intensity. Hence greater benefits of an OPX are realized by hospitals with high CMI or high resident intensity. This estimate offers the first empirical evidence to the efficacy of these administrative innovations. The significance of these improvements in HCAHPS are better highlighted when compared to only a 0.85% annual improvement in HCAHPS for hospitals that did not have an OPX.
Given the effectiveness of OPXs in improving HCAHPS, we conducted additional analyses to investigate the cost of implementing these offices. We find that the operating costs, which include expenses incurred in every aspect of a hospital’s operations, reduce by 1.4% for each year of its existence. These are also sizable improvements in operating efficiencies, especially given the low margins of operation for a vast majority of hospitals – the median operating margin for hospitals in 2018 was 1.7% .
Finally, taking cues from our interviews with the OPX and hospital staff at a prominent teaching hospital, we also investigated the impact of the background of the CXO (medical vs. non-medical) on the effectiveness of an OPX. In our dataset, we find that only a small proportion of the CXOs (14.5%) had a medical background, i.e., a nursing (RN, BSN) or MD/DO degree. Preliminary evidence suggests that a CXO with a medical background is more effective at improving EQ than a non-medical CXO. Specifically, a hospital with a medical CXO observes a 1.6% improvement in HCAHPS, compared to a 0.1% improvement in HCAHPS for a non-medical CXO, with each year of OPX operation. This suggests an interesting managerial insight on how to lead these offices in a hierarchical industry such as healthcare. Taken together, these results offer preliminary insights on the role and efficacy of these new administrative innovations in the healthcare industry. It also offers important policy implications to CMS on how to prioritize and manage HCAHPS.